Summary
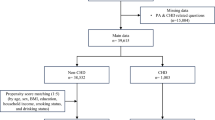
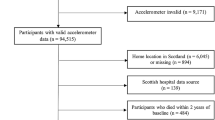
The intervention of behaviors, including physical activity (PA), has become a strategy for many hospitals dealing with patients with chronic diseases. Given the limited evidence available about PA and healthcare use with chronic diseases, this study explored the association between different levels of PA and annual hospital service use and expenditure for inpatients with coronary heart disease (CHD) in China. We analyzed PA information from the first follow-up survey (2013) of the Dongfeng-Tongji cohort study of 1460 CHD inpatients. We examined factors such as PA exercise volume and years of PA and their associations with the number of inpatient visits, number of hospital days, and inpatient costs and total medical costs. We found that the number of hospital days and the number of inpatient visits were negatively associated with intensity of PA level. Similarly, total inpatient and outpatient costs declined when the PA exercise volume levels increased. Furthermore, there were also significant associations between the number of hospital days, inpatient costs or total medical costs and levels of PA years. This study provides the first empirical evidence about the effects of the intensity and years of PA on hospital service use and expenditure of CHD in China. It suggests that the patients’ PA, especially the vigorous PA, should be promoted widely to the public and patients in order to relieve the financial burden of CHD.
Similar content being viewed by others
References
Hamer M, de Oliveira C, Demakakos P. Non-exercise physical activity and survival: English Longitudinal Study of Ageing. Am J Prev Med, 2014, 47(4): 452–460
Martínez-Gómez D, Guallar-Castillón P, León-Muñoz LM, et al. Household physical activity and mortality in older adults: a national cohort study in Spain. Prev Med, 2014, 61: 14–19
Chen H, Huang N, Li WJ, et al. Clinical and laboratory features, and quality of life assessment in wheat dependent exercise-induced anaphylaxis patients from central China. J Huazhong Univ Sci Technolog Med Sci, 2016, 36(3): 410–415
Jefferis BJ, Whincup PH, Lennon LT, et al. Physical activity in older men: longitudinal associations with inflammatory and hemostatic biomarkers, N-terminal pro-brain natriuretic peptide, and onset of coronary heart disease and mortality. J Am Geriatr Soc, 2014, 62(4): 599–606
Chomistek AK, Manson JE, Stefanick ML, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women’s Health Initiative. J Am Coll Cardiol, 2013, 61(23): 2346–2354
Booth FW, Gordon SE, Carlson CJ, et al. Waging war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol, 2000, 88(2): 774–787
Kohl HW 3rd, Craig CL, Lambert EV, et al. Lancet Physical Activity Series Working Group. The pandemic of physical inactivity: global action for public health. Lancet, 2012, 380(9838): 294–305
Sari N. Exercise, physical activity and healthcare utilization: A review of literature for older adults. Maturitas, 2011, 70(3): 285–289
Simmonds B, Fox K, Davis M, et al. Objectively assessed physical activity and subsequent health service use of UK adults aged 70 and over: a four to five year follow up study. PLoS One, 2014, 9(5): e97676
Fisher KL, Harrison EL, Reeder BA, et al. Is self-reported physical activity participation associated with lower health services utilization among older adults? Cross-sectional evidence from the canadian community health survey. J Aging Res, 2015: 425354
Vegda K, Nie JX, Wang L, et al. Trends in health services utilization, medication use, and health conditions among older adults: a 2-year retrospective chart review in a primary care practice. BMC Health Serv Res, 2009, 9: 217
Lankenau B, Solari A, Pratt M. International physical activity policy development: a commentary. Public Health Rep, 2004, 119(3): 352–355
Bauman A, Finegood DT, Matsudo V. International perspectives on the physical inactivity crisis-structural solutions over evidence generation? Prev Med, 2009, 49(4): 309–312
Rütten A, Abu-Omar K, Gelius P, et al. Policy assessment and policy development for physical activity promotion: results of an exploratory intervention study in 15 European nations. Health Res Policy Syst, 2012, 10: 14
Global atlas on cardiovascular disease prevention and control: Policies, strategies and interventions [http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/]
Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health, 2011, 32: 39–69
Codogno JS, Turi BC, Kemper HC, et al. Physical inactivity of adults and 1-year health care expenditures in Brazil. Int J Public Health, 2015, 60(3): 309–316
Arredondo A, Zúñiga A, Parada I. Health care costs and financial consequences of epidemiological changes in chronic diseases in Latin America: evidence from Mexico. Public Health, 2005, 119(8): 711–720
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2018, 392(10159): 1736–1788
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2018, 392(10159): 1789–1858
Dou L, Liu X, Zhang T, et al. Health care utilization in older people with cardiovascular disease in China. Int J Equity Health, 2015, 14: 59
Wu F, Guo Y, Kowal P, et al. Prevalence of major chronic conditions among older Chinese adults: the Study on Global AGEing and adult health (SAGE) wave 1. PLoS One, 2013, 8(9): e74176
Wang F, Zhu J, Yao P, et al. Cohort Profile: the Dongfeng-Tongji cohort study of retired workers. Int J Epidemiol, 2013, 42(3): 731–740
Tian C, Huang Q, Yang L, et al. Green tea consumption is associated with reduced incident CHD and improved CHD-related biomarkers in the Dongfeng-Tongji cohort. Sci Rep, 2016, 6: 24353
Cannon CP, Battler A, Brindis RG, et al. American College of Cardiology key data elements and definitions for measuring the clinicalmanagement and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute CoronarySyndromes Writing Committee). J Am Coll Cardiol, 2001, 38(7): 2114–2130
Chen M, He M, Min X, et al. Different physical activity subtypes and risk of metabolic syndrome in middle-aged and older Chinese people. PLoS One, 2013, 8(1): e53258
Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc, 2011, 43: 1575–1581
Liu-Ambrose TYL, Ashe MC, Marra C, et al. Independent and inverse association of healthcare utilisation with physical activity in older adults with multiple chronic conditions. Br J Sports Med, 2010, 44(14): 1024–1028
Sari N. A short walk a day shortens the hospital stay: physical activity and the demand for hospital services for older adults. Can J Public Health, 2010, 101(5): 385–389
Liu-Ambrose TY, Ashe MC, Marra C, et al. Independent and inverse association of healthcare utilization with physical activity in older adults with multiple chronic conditions. Br J Sports Med, 2010, 44(14): 1024–1028
Woolcott JC, Ashe MC, Miller WC, Shi P, Marra CA; PACC Research Team. Does physical activity reduce seniors’ need for healthcare? A study of 24 281 Canadians. Br J Sports Med. 2010, 44(12): 902–904.
Janssen I. Health care costs of physical inactivity in Canadian adults. Appl Physiol Nutr Metab, 2012, 37(4): 803–806
Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis, 2015, 57(4): 315–523
Kadoglou NP, Iliadis F, Angelopoulou N, et al. Cardiorespiratory capacity is associated with favourable cardiovascular risk profile in patients with Type 2 diabetes. J Diabetes Complications, 2009, 23(3): 160–166
Zanesco A, Antunes E. Effects of exercise training on the cardiovascular system: pharmacological approaches. Pharmacol Ther, 2007, 114(3): 307–317
Craft LL, Perna FM. The Benefits of Exercise for the Clinically Depressed. Prim Care Companion J Clin Psychiatry, 2004, 6(3): 104–111
Verhaak PF, Heijmans MJ, Peters L, et al. Chronic disease and mental disorder. Soc Sci Med, 2005, 60(4): 789–797
Bassuk SS, Manson JE. Physical activity and cardiovascular disease prevention in women: a review of the epidemiologic evidence. Nutr Metab Cardiovasc Dis, 2010, 20(6): 467–473
Reddigan JI, Ardern CI, Riddell MC, et al. Relation of physical activity to cardiovascular disease mortality and the influence of cardiometabolic risk factors. Am J Cardiol, 2011, 108(10): 1426–1431
Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation, 2010, 122(7): 743–752
Ku PW, Fox KR, Gardiner PA, et al. Late-life exercise and difficulty with activities of daily living: an 8-year nationwide follow-up study in Taiwan. Ann Behav Med. 2016, 50(2): 237–246
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001, 56(3): M146–M156
Zhang Q, Zhao D, Xie W, et al. Trends in length of hospital stay and in-hospital cost for coronary heart disease from 2007 to 2012 in Beijing. Xinfei Xueguanbing Zazhi (Chinese), 2016, 35(2): 75–80
Wang Z, Jiang L, Zhu J, et al. The effect of nutritional status of the patients with coronary heart disease on their hospital days. Zhongguo Laonian Xinxueguan Jibing (Chinese). 2016, 18(4): 384–387
Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet, 2012, 379(9818): 805–814
Barber SL, Borowitz M, Bekedam H, et al. The hospital of the future in China: China’s reform of public hospitals and trends from industrialized countries. Health Policy Plan, 2014, 29(3): 367–378
Hallal PC, Andersen LB, Bull FC, et al. Lancet Physical Activity Series Working Group. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet, 2012, 380(9839): 247–257
Barnett I, van Sluijs E, Ogilvie D, et al. Changes in household, transport and recreational physical activity and television viewing time across the transition to retirement: longitudinal evidence from the EPIC-Norfolk cohort. J Epidemiol Community Health, 2014, 68(8): 747–753
American College of Sports Medicine, Chodzko-Zajko WJ, Proctor DN, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc, 2009, 41(7): 1510–1530
Eurobarometer, Special Eurobarometer. 183-6/Wave 58.2-European Opinion Research Group EEIG. Physical Activity. Retrieved May 16, 2019 from: http://ec.europa.eu/commfrontoffice/publicopinion/archives/ebs/ebs_183_6_en.pdf
Li LW, Long Y, Essex EL, et al. Elderly Chinese and their family caregivers’ perceptions of good care: A qualitative study in Shandong, China. J Gerontol Soc Work, 2012, 55(7): 609–625
Su C, Jia XF, Wang ZH, et al. Longitudinal association of leisure time physical activity and sedentary behaviors with body weight among Chinese adults from China Health and Nutrition Survey 2004–2011. Eur J Clin Nutr, 2017, 71(3): 383–388
Clark AM, DesMeules M, Luo W, et al. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol, 2009, 6(11): 712–722
Janković J, Erić M, Stojisavljević D, et al. Socio- Economic Differences in Cardiovascular Health: Findings from a Cross-Sectional Study in a Middle- Income Country. PLoS One, 2015, 10(10): e0141731
Rocca P, Beckman A, Ekvall Hansson E, et al. Is the association between physical activity and healthcare utilization affected by self-rated health and socio-economic factors? BMC Public Health, 2015, 15: 737
Acknowledgments
We thank all study participants and staff of the Health Examination Center of the Dongfeng Central Hospital and the Medical Insurance Center of DMC for their generous help. We also thank the interviewers from the retirement management office of DMC and from Tongji Medical College, HUST. The Dongfeng-Tongji Cohort Study is a collaboration among the Tongji Medical College, Huazhong University of Science and Technology, the DMC and the Harvard School of Public Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by China Medical Board and the Fundamental Research Funds for the Central Universities, HUST (No. 2015XJGH014).
Rights and permissions
About this article
Cite this article
Wang, F., Zhang, Ly., Zhang, P. et al. Effect of Physical Activity on Hospital Service Use and Expenditures of Patients with Coronary Heart Disease: Results from Dongfeng-Tongji Cohort Study in China. CURR MED SCI 39, 483–492 (2019). https://doi.org/10.1007/s11596-019-2063-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-019-2063-x