Abstract
Background
Costs of informal care are ignored in many cost-effectiveness analyses (CEAs) conducted from a societal perspective; however, these costs are relevant for lifesaving interventions targeted at the older population. In this study, we estimated informal care costs by age and proximity to death across European regions and showed how these estimates can be included in CEAs.
Methods
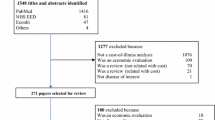
We estimated informal care costs by age and proximity to death using generalised linear mixed-effects models. For this, we selected deceased singles from the Survey of Health, Ageing and Retirement, which we grouped by four European regions. We combined the estimates of informal care costs with life tables to illustrate the impact of including informal care costs on the incremental cost-effectiveness ratio (ICER) of a hypothetical intervention that prevents a death at different ages.
Results
Informal care use, and hence informal care costs, increase when approaching death and with increasing age. The impact of including informal care costs on the ICER varies between €200 and €17,700 per quality-adjusted life-year gained. The impact increases with age and is stronger for women and in southern European countries.
Conclusion
Our estimates of informal care costs facilitate including informal care costs in CEAs of life-extending healthcare interventions. Including these costs may influence decisions as it leads to reranking of life-extending interventions compared with interventions improving quality of life.
Similar content being viewed by others
Informal care use, and hence informal care costs, increase when approaching death and with increasing age. |
The impact of including informal care costs on the incremental cost-effectiveness ratio of a hypothetical intervention that prevents a death at different ages varies between €200 and €17,700 per quality-adjusted life-year gained. |
Our findings can be used to include the costs of informal care in economic evaluations of life-extending health care interventions, which may improve health care decision making. |
1 Introduction
Informal care costs are substantial: 0.9–5.0% of the Gross Domestic Product in European countries [1]. Many new medical interventions are targeted at older people with chronic diseases such as cardiovascular disease and respiratory disease. Some of these interventions improve survival, thereby also influencing the demand for informal care during the added life-years. However, cost-effectiveness analyses (CEAs) mostly include public expenditures while ignoring the costs of informal care [2]. As a result, the total costs of these interventions are underestimated. Consequently, the incremental cost-effectiveness ratio (ICER) of interventions that increase the burden on informal caregivers looks more favourable than it is.
The impact of health care interventions often goes beyond the health care sector. For this reason, CEAs should not only consider the impact of an intervention on the costs within the health care sector but also its costs elsewhere in society [3, 4]. Pharmacoeconomic guidelines such as the Dutch guidelines therefore stipulate including the costs of informal care [5]. However, these costs are still ignored in most CEAs [2] because data on informal care use are often not collected when evaluating specific interventions. Consequently, the impact of a health care intervention on informal care use is unknown.
Standardised methods facilitate the inclusion of many relevant costs, e.g. unrelated medical costs and costs of non-medical consumption in life-years gained [6,7,8]. A standardised method to include estimates of informal care costs might overcome the issue of data availability. This study therefore estimates the relationship between informal care use and age and proximity to death. These are known predictors of health, and data are readily available in most (modelling) studies that evaluate a health care intervention. This means that our estimates can be used in a standardised way to include informal care costs in CEAs when estimating the cost effectiveness of life-prolonging interventions.
A simple way to include informal care costs in cost-effectiveness studies would be to use estimates of informal care costs by age. Such an approach has been applied when estimating the costs of medical and non-medical consumption of life-prolonging interventions [9, 10]. However, studies on the relationship between age and health care spending suggest this approach would overestimate the costs of life-extending interventions [11]. Average health care spending increases with age, yet this increase is, to a large extent, because at higher ages a larger proportion of the population is in poor health and closer to death. As life-extending interventions increase the share of people alive at older ages, they are thus expected to shift the age profile of health care spending to the right. Some evidence even suggests that lifetime costs decrease because expenditures in the last year of life decrease with age [12, 13]. Additionally, when costs are shifted to later ages, their present value decreases, which lowers their impact on the cost-effectiveness ratio [14].
To capture the effect of mortality on the age profile of health care spending, Zweifel et al. proposed to estimate health care spending as a function of both age and proximity to death [15]. Once controlling for time to death, the age profile of health care spending becomes almost flat. Since then, many studies have confirmed that the relation between health care spending and age can (at least partially) be explained by proximity of death. This is supported by the finding that health losses and disability are more pronounced in the last years of life [16, 17]. Most of these studies focused on hospital care or medical care [18,19,20]. Research on formal long-term care also found a relation between proximity to death and spending [11, 21,22,23,24], although the effect of time to death is less strong than in curative care and a significant role of age seems to remain [11, 24].
Although Balia and Brau [25] found a relationship between informal care and proximity to death after controlling for formal long-term care (i.e. paid domestic help), this relationship has been less extensively studied. In this study, we also estimate the relationship between informal care use and age and proximity to death. We do this using longitudinal survey data from single persons in 28 European countries and Israel. The analyses are stratified by region, as the extent to which informal care substitutes for formal care depends on the comprehensiveness of (social) insurance for long-term care and on institutional and cultural differences [26]. By using proximity to death to predict informal care use, we capture the fact that life-prolonging interventions might lead to a postponement of some informal care use. Much informal care use that is used in the years directly preceding death is postponed to higher ages by postponing death. We move beyond prior research by using these estimates to generate profiles of the costs of informal care by age and proximity to death that can be linked to any health economic model that predicts survival.
2 Methods
We estimated annual informal care use as a function of age, gender and proximity to death using data from singles participating in the Survey of Health, Ageing and Retirement in Europe (SHARE) [27, 28]. We produced separate estimates for northern, western, southern and eastern European countries. Finally, we illustrate the impact of including informal care costs on the ICER using a hypothetical intervention that prevents a death at different ages.
2.1 Data and Descriptive Statistics
The SHARE survey collects longitudinal data on health, socioeconomic status and social and family networks of non-institutionalised people aged over 50 years in 28 European countries and Israel. Waves 1 and 2 and 4–8 (from 2004 to 2020) are used in this analysis (release 7.1.0 of waves 1–6, release 7.1.1 of wave 7 and release 1.0.0 of wave 8) [29,30,31,32,33,34,35]. The focus of the third wave was on life history, which cannot be compared or linked to the questions of the other waves. Data from wave 8 were only used to supplement the information on death.
Respondents were asked to describe the frequency of informal care received (almost daily, almost every week, almost every month, or less often) from a family member from outside the household, any friend or neighbor with personal care, the household or paperwork, as well as the average number of hours (per day, week, month and year) of informal care received. The latter was asked only in waves 1 and 2. Respondents were also asked to describe whether regular help with personal care was received from someone living within the household. We defined informal care use as a dummy indicator for whether the individual has received informal care from outside the household at least weekly or regular help from someone living within the household, and build a continuous variable for the number of hours of informal care received per day.Footnote 1
In waves 1, 2, 4 and 5, the answer on informal care received from outside the household refers to either the respondent or to his/her husband, wife or partner, or to both of them. Therefore, the sample was restricted to individuals who were single across all waves in order to correctly assess the person within a household who received informal care, i.e. the person him or herself instead of his/her husband, wife or partner. The sample was further restricted to individuals with complete data, including a date of death, in order to calculate proximity to death for all individuals. This resulted in 12,239 observations for over 6100 participants.
Table 1 shows the distribution of responder’s characteristics by wave. In 40.2% of the observations, participants responded to have received informal care from outside the household by a family member, friend, or neighbor at least weekly, or responded to have received regular help from someone from within the household in the 12 months prior to the interview.
The probability of using informal care at least weekly increased with age (55.3% among those aged 85+ years) (Fig. 1a) and proximity to death (51.6% among those who died in the same year of the interview) (Fig. 1b). The daily number of hours of informal care use among those who indicated to use informal care at least weekly tends to increase with age (3.3 h/day among those aged 85+ years; SD: 4.1) (Fig. 1c) and with proximity to death (4.4 h/day among those who died in the same year of the interview; SD: 6.5) (Fig. 1d).
Informal care use: proportion of users and mean number of hours per day (standard deviation) by a, c age and b, d proximity to death. Standard deviation for proportions in Fig. 1a and b are < 0.01
2.2 Model Specification
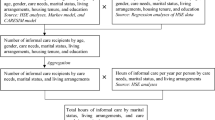
To include informal care costs in cost-effectiveness studies, we needed to estimate both the probability of any use and the (conditional) number of hours used as a function of proximity to death, age and gender. We used a two-step approach. First, we estimated the probability of using informal care at least weekly, and second, we estimated the daily number of hours of informal care use among persons who used informal care. This approach is in line with previous studies [18, 20]. In both models, we included gender, age and proximity to death as predictors. Proximity to death was calculated as the difference between month and year of death and month and year of the interview.
For the first step, logistic random effects regression analyses were employed to estimate the probability of using informal care at least weekly. To grasp the importance of the inclusion of proximity to death in explaining informal care use, we first estimated a model only including gender and age as explanatory variables. In a second model, we then added proximity to death. A comparison of the age profiles in the two models provided an indication of how much of the relation between informal care use and age observed in a simple model is caused by the strong correlation between age and death. The resulting models are shown in Eqs. 1 and 2:
where p is the probability of informal care use at least weekly; αi is the subject-specific intercept (random-effect); A is the responder age; A2 is age squared; S is the responder sex; TTD is the time to death; i is the index of the individual; and t is the index of the wave.
For the second step, the same explanatory variables were used to estimate the number of daily hours of informal care. As this outcome is a count variable, negative binomial regression models were used. The quadratic term of age was not significant, indicating that the relationship between age and number of informal care hours was not curvilinear and therefore it was not included in Eqs. 3 and 4.
While wave 1 and 2 from SHARE contained information on the number of hours of informal care use from outside the household, this information was no longer available in subsequent waves. These latter two models were therefore based on data from waves 1 and 2 only.
The relationship between informal care use and functional limitations strongly differs across countries, as it depends on cultural norms and public policy that influence the availability of (publicly subsidised) long-term care [25, 36]. Since proximity to death is strongly correlated with functional limitations [24], it is likely that the relationship between proximity to death and informal care use is also influenced by culture and public policy. All analyses were therefore stratified by European region. In line with Bolin et al. [26], we distinguished between northern, western and southern European countries and added eastern European countries. The countries included within these regions were: northern Europe (Finland, Denmark, Sweden), western Europe (Austria, France, Germany, Ireland, Switzerland, Belgium, Luxemburg, and Netherlands), southern Europe/Mediterranean area (Spain, Greece, Portugal, Cyprus, Malta, Israel and Italy) and eastern Europe (Czech Republic, Poland, Hungary, Slovenia, Estonia, Croatia, Lithuania, Bulgaria, Latvia, Romania, Slovakia).
2.3 Estimation of Hours of Informal Care Use and the Impact on the Incremental Cost-Effectiveness Ratio (ICER)
We subsequently estimated weekly hours of informal care use for the different European regions by combining the probability of using informal care at least weekly (using Eq. 2) and the daily number of hours of informal care use (using Eq. 4) given certain ages and proximity death, separately for men and women.
We valued informal care with country-specific standard rates of formal caregivers providing similar activities, namely: Sweden for northern Europe (€16.63/h), The Netherlands for western Europe (€13.79/h), Spain for southern Europe (€11.24/h) and Hungary for eastern Europe (€4.06/h) [1]. Prices were inflated to 2021 levels [37]. To evaluate the impact of including informal care costs on the ICER, we followed the approach by Kellerborg et al. [38]. An ICER that considers informal care costs, besides the costs within health care and the costs within other sectors, is calculated as shown in Eq. 5:
where the last term represents the effect on the ICER of including the costs of informal care. We estimated this effect by using a hypothetical intervention that prevents a death at different ages without any intervention costs (reducing Eq. 5 to the last term only). To estimate the impact on the ICER of the costs of informal care for an intervention that prevents a death at age a, we use the following equation (Eq. 6):
where the numerator equals the informal care costs at a given age a and TTD t multiplied by \(L(a,t)\), which is the number of people alive at a given age a and TTD t, summed over age (denoted by the index a) and TTD (denoted by the index t). The denominator is the average quality of life at age \(a\) multiplied by the number of people alive at age a, summed over all ages. The ICERs as calculated using Eq. 6 can be interpreted as the cost effectiveness of a hypothetical intervention in which a death at a certain age is prevented at zero intervention costs. Previous research has shown that such ICERs give a good indication of what the impact is of including future costs on the ICER of non-hypothetical interventions [7, 9].
Estimates of \(L\left(a\right)\) and \(L\left(a,t\right)\) are based on a life table, and on 1-year mortality rates obtained from the Human Mortality Database [39]. Life tables for The Netherlands (2020), Spain (2018), Sweden (2019) and Hungary (2020) were used for western, southern, northern and eastern European countries, respectively [39]. Age-specific estimates of \(\mathrm{QoL}\left(a\right)\) were derived from country-specific individual-level EQ-5D survey data, but using the Dutch value set [40]. The impact of the costs of informal care was estimated separately for ages 50–90 years, and separately for men and women, taking a lifetime time horizon. Future costs and quality-adjusted life-years (QALYs) were discounted according to the country-specific discount rates [41].
To take into account the uncertainty of the parameters that are used to estimate the probability of using informal care at least weekly and the hours of informal care use per day, we conducted a probabilistic sensitivity analysis by drawing regression parameters randomly from multivariate normal distributions derived from the variance-covariance matrixes of the two regression equations for use and conditional hours. We report the average incremental costs and the average incremental costs per life-year and QALY gained across all 1000 runs.
3 Results
3.1 Regression Models
Tables 2 and 3 present the results of the models estimating the probability of informal care use at least weekly and the conditional hours of informal care use by gender, age, and proximity to death, stratified by European region.
Model 1 (Table 2) shows a relationship between age and informal care use in western European countries, indicating that the probability of using informal care at least weekly increases with age. Model 1 also shows that women more often use informal care than men. For example, the probability of a 50-year-old woman using informal care at least weekly is estimated to be 9%, while for a 90-year-old woman is estimated to be 50%. In the case of a 50-year-old man, the probability of using informal care at least weekly is estimated to be 7%, while for a 90-year-old man is estimated to be 42%. Model 2 (Table 2) shows a significant relationship between proximity to death and informal care use in western European countries, indicating that informal care use increases when someone approaches death, but there is a separate role of age in addition to proximity to death. For example, the probability of a 70-year-old woman using informal care at least weekly is estimated to be 16% when 10 years prior to death, but 25% when dying in the same year.
Proximity to death is also a strong predictor of the daily number of hours of informal care use received in western European countries, but again there is a separate role for age (Model 4, Table 3). For example, a 70-year-old woman would need about 1 hour/day of informal care when 10 years prior to death, but about 3 hours/day when dying in the same year.
Similar to western European countries, there is a relationship between both age and proximity to death and the probability of using informal care at least weekly in the other European regions.
Figure 2 shows the predicted informal care hours per week for men and women by age and proximity to death, across European regions, based on the combination of model (2) and model (4). From these figures, we can see most clearly the age and proximity to death patterns of informal use and how these vary by region. The weekly hours of informal care were highest in eastern European countries, followed by the southern European countries. The lowest number of weekly hours of informal care were reported in the northern European countries. In all European regions, the number of hours/week of informal care increased by age and proximity to death.
3.2 Informal Care Costs and Impact on the ICER
Table 4 shows the impact of including informal care costs on the ICER of a hypothetical intervention that prevents a death at different ages, across European countries. Discounted incremental costs increase with age. For example, in western European countries, these costs increase from €9300 (SD €400) to €20,300 (SD €1900) for men, and from €14,400 (SD €400) to €30,000 (SD €1500) for women from age 50 years to 90 years. The impact on the ICER in western European countries varies from €400 to €6200 for men, and from €600 to €8600 for women, depending on age. The impact on the ICER is highest in southern European countries. Within these countries, the impact on the ICER varies from €1600 to €14,200 for men, and from €2300 to €17,700 for women. Interestingly, the impact on the ICER is much stronger in southern European countries than in western and northern European countries even though the value per hour is lower in these countries.
4 Discussion
Economic evaluations of healthcare interventions that adopt a societal viewpoint need to include the costs of informal care. These costs are often ignored, in part because data on informal care use is not collected when evaluating specific interventions or diseases. We therefore generated cost profiles built using prediction models with age, gender and proximity to death as predictors to facilitate the inclusion of informal care costs in CEAs of life-extending interventions across different European countries. We found that weekly informal care use, and hence informal care costs, increase with age and when approaching death, and vary across countries. The impact on the ICER strongly depends on age and gender and varies from €400 to €8600 in western European countries and from €1600 to €17,700 in southern European countries.
4.1 Relation with the Literature on Time to Death
Our study extends the literature on the relationship between age, proximity to death, and informal care use by Balia and Brau [25]. Our results are in line with theirs and we extend their analysis by including more waves and more countries, and by generating informal care cost profiles by age, proximity to death and European region. These profiles may be used in CEAs of healthcare interventions and thus contribute to a more complete estimate of the incremental cost-effectiveness of these interventions.
A role of proximity to death in explaining the age pattern in health care spending has been found in almost all studies. However, the magnitude of the effect differs widely across different types of expenditures: expenditures in hospital care depend on proximity to death rather than age, while in long-term care age and disability seem to play a distinct role from mortality [11]. These differences are related to the different aims (curing versus caring) and the relevance of different dimensions of health, of which not all have the same relation with mortality (prevalence of [lethal] diseases versus functioning and disability). Our results show that proximity to death is an important predictor of informal care use, but that a separate role for age remains. Given that informal care has, to some extent, similar aims as formal long-term care, and both forms of care are to some extent substitutes [42], these results are in line with expectations.
4.2 Relation with Earlier Work on Informal Care Costs in CEAs
Gheorghe et al. also aimed to overcome the poor availability of informal care data by predicting informal care use with data that are often available to health economic researchers [43]. In contrast to our approach, they used EQ-5D scores of patients to estimate informal care use. We think our approach is complementary to theirs, with their estimates being useful in studies where interventions do not extend life (i.e. interventions that only or also have a strong impact on morbidities that are less lethal), while our estimates are useful in studies of interventions that extend life.
Ideally, the burden on informal caregivers in terms of the time spent on caregiving is measured using a diary in which caregivers record the time they spend on caregiving, or using a questionnaire where caregivers are retrospectively asked about the time spent on care tasks [44]. However, data from these sources are not always available when evaluating specific interventions or diseases. If data are available for instance from a trial with a short follow-up, these can be combined with our estimates if a model is used to extrapolate findings from that trial in a cost-effectiveness study. More generally, frameworks are available to combine more detailed cost data from other studies with estimates such as presented in this paper that represent averages per capita instead of estimates for specific patient groups [7, 45].
Traditionally, researchers either use foregone wages or the wage rate of a formal caregiver to assess opportunity costs. Many informal caregivers are retired and hence foregone wages based on the respondent’s wage or the wages of those with a similar age likely underestimate these opportunity costs because many have zero earnings. Because we only knew the caregiver’s relation to the recipient of care and, in the case of children, their age and gender, we were unable to value informal care using the wage rate of the informal carer on the labour market. Hence, we used the proxy good method to estimate the costs of informal care to give insight into the possible impact of including informal care costs on the ICER. Others who use our estimates of informal care use by age and time to death can value informal care differently, for example by using wage rates when this information is available to them.
Another strand of research studied how to measure care-related quality of life in informal caregivers [46, 47], and how to value the outcomes to include care-related quality of life in CEAs [47, 48]. While such studies are relevant and promising, including the impact of informal care in CEAs on the cost side seems more straightforward.
4.3 Comparison with the Impact of Other Cost Categories on the ICER
Similar to our approach, standardised methods have been developed to facilitate the inclusion of unrelated medical costs and costs of non-medical consumption in life-years gained in CEAs [6, 7]. Mokri et al. estimated future medical and non-medical costs and their impact on the ICER of life-prolonging interventions across five European countries [8]. They found that future medical costs in The Netherlands, Germany and the UK are large compared with future medical costs in Spain and Greece. Conversely, we found that informal care use in western European countries, including The Netherlands and Germany, are low compared with southern European countries, including Spain and Greece. A possible explanation for this difference is that formal and informal care are to some extent substitutes [26]. Consequently, the impact of including informal care costs compared with the impact of including future medical costs on the ICER of a hypothetical intervention that prevents a death at different ages is higher in Spain but lower in The Netherlands. For example, Mokri et al. found that the impact of including future medical costs on the ICER of a hypothetical intervention that prevents a death at age 75 years in Spain or The Netherlands is estimated to be €4900 or €18,800, respectively [8]. In comparison, we estimated that the impact of including informal care costs on the ICER of a hypothetical intervention that prevents a death at age 80 years is €8200 in men and €10,700 in women in southern European countries, and €3100 in men and €4500 in women in western European countries.
4.4 Limitations
This study is subject to several limitations related to the data. First, the number of cases with complete information on date of death and informal care receipt is only 3.6% (12,239 of 336,601) because of incomplete information about informal care within the household, and because the exit interview after death with relatives was available only in a few cases. A consequence of the incomplete information about informal care within the household was that we had to rely on data from singles only, while singles tend to have poorer health than couples. We believe this is not necessarily a problem if these effects are captured by the proxies for health in the models (age and TTD). Furthermore, the undersampling of people in a nursing home is a limitation. Together, these data limitations mean that the data are likely not representative for the full populations of the countries that we included. However, since the number of single adult households is increasing in the European Union [49], singles are an important group to analyse for policy purposes.
A further limitation is that while waves 1 and 2 from SHARE contained information on the number of hours of informal care from outside the household, this information was no longer available in subsequent waves, and we had to assume that this information from the first two waves is representative for help from outside and inside the household in subsequent waves.
5 Conclusion
Our findings can be used to include the costs of informal care in economic evaluations of life-extending health care interventions when data on informal care use by disease are lacking. Since our estimates are not disease-specific, they are probably most useful in studies of interventions that extend life. They are easy to incorporate in any health economic model of the cost effectiveness of health care interventions that predicts survival and incorporates data on the number of people who have died over time. Including these costs will have a large impact and will lead to reranking of life-extending interventions compared with interventions that improve quality of life.
Notes
Due to poor accuracy in the responses, those individuals who reported having received more than 16 h of care per day have been set to 16 h of care from each helper.
References
European Commission. Study on exploring the incidence and costs of informal long-term care in the EU. European Commission; 2021.
Krol M, Papenburg J, van Exel J. Does including informal care in economic evaluations matter? A systematic review of inclusion and impact of informal care in cost-effectiveness studies. Pharmacoeconomics. 2015;33:123–35.
Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Gold M, Siegel J, Russell L, et al. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 1996.
Zorginstituut Nederland (Dutch National Health Care Institute). Richtlijn Voor Het Uitvoeren van Economische Evaluaties in de Gezondheidzorg (Guideline for the Conduct of Economic Evaluations in Healthcare). Dutch National Health Care Institute; 2016.
van Baal PH, Wong A, Slobbe LC, et al. Standardizing the inclusion of indirect medical costs in economic evaluations. Pharmacoeconomics. 2011;29:175–87.
Kellerborg K, Perry-Duxbury M, de Vries L, et al. Practical Guidance for Including Future Costs in Economic Evaluations in The Netherlands: Introducing and Applying PAID 3.0. Value Health. 2020;23:1453–61.
Mokri H, Kvamme I, de Vries L, et al. Future medical and non-medical costs and their impact on the cost-effectiveness of life-prolonging interventions: a comparison of five European countries. Eur J Health Econ. 2022. https://doi.org/10.1007/s10198-022-01501-6.
Meltzer D. Accounting for future costs in medical cost-effectiveness analysis. J Health Econ. 1997;16:33–64.
de Vries LM, van Baal Pieter HM, Brouwer WBF. Future costs in cost-effectiveness analyses: past, present, future. Pharmacoeconomics. 2019;37:119–30.
de Meijer C, Wouterse B, Polder JJ, et al. The effect of population aging on health expenditure growth: a critical review. Eur J Ageing. 2013;10:353–61.
Levinsky NG, Yu W, Ash A, et al. Influence of age on Medicare expenditures and medical care in the last year of life. JAMA. 2001;286:1349–55.
Yang Z, Norton EC, Stearns SC. Longevity and health care expenditures: the real reasons older people spend more. J Gerontol B Psychol Sci Soc Sci. 2003;58:S2-10.
Gandjour A, Lauterbach KW. Does prevention save costs? Considering deferral of the expensive last year of life. J Health Econ. 2005;24:715–24.
Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ. 1999;8:485–96.
Gheorghe M, Brouwer WBF, van Baal PHM. Health losses at the end of life: a Bayesian mixed beta regression approach. J R Statist Soc. 2017;180:723–49.
Majer IM, Nusselder WJ, Mackenbach JP, et al. Mortality risk associated with disability: a population-based record linkage study. Am J Public Health. 2011;101:e9–15.
Seshamani M, Gray AM. A longitudinal study of the effects of age and time to death on hospital costs. J Health Econ. 2004;23:217–35.
Wong A, van Baal PH, Boshuizen HC, et al. Exploring the influence of proximity to death on disease-specific hospital expenditures: a carpaccio of red herrings. Health Econ. 2011;20:379–400.
Werblow A, Felder S, Zweifel P. Population ageing and health care expenditure: a school of “red herrings”? Health Econ. 2007;16:1109–26.
Weaver F, Stearns SC, Norton EC, et al. Proximity to death and participation in the long-term care market. Health Econ. 2009;18:867–83.
Wong A, Kommer GJ, Polder JJ. Levensloop en zorgkosten. Solidariteit en de zorgkosten van vergrijzing. Report from the National Institute for Public Health and the Environment 270082001. 2008.
de Meijer CA, Majer IM, Koopmanschap MA, et al. Forecasting lifetime and aggregate long-term care spending: accounting for changing disability patterns. Med Care. 2012;50:722–9.
de Meijer C, Koopmanschap M, D’Uva TB, et al. Determinants of long-term care spending: age, time to death or disability? J Health Econ. 2011;30:425–38.
Balia S, Brau R. A country for old men? Long-term home care utilization in Europe. Health Econ. 2014;23:1185–212.
Bolin K, Lindgren B, Lundborg P. Informal and formal care among single-living elderly in Europe. Health Econ. 2008;17:393–409.
Borsch-Supan A, Brandt M, Hunkler C, et al. Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013;42:992–1001.
Bergmann M, Kneip T, De Luca G, et al. Survey participation in the Survey of Health, Ageing and Retirement in Europe (SHARE), Wave 1-7. Based on Release 7.0.0. SHARE Working Paper Series 41-2019. Munich: MEA, Max Planck Institute for Social Law and Social Policy; 2019.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 1. Release version: 7.1.0. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w1.710.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 2. Release version: 7.1.0. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w2.710.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 4. Release version: 7.1.0. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w4.710.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 5. Release version: 7.1.0. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w5.710.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 6. Release version: 7.1.0. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w6.710.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 7. Release version: 7.1.1. SHARE-ERIC. Data set. 2020. https://doi.org/10.6103/SHARE.w7.711.
Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. Release version: 1.0.0. SHARE-ERIC. Data set. 2021. https://doi.org/10.6103/SHARE.w8.100.
Bakx P, de Meijer C, Schut F, et al. Going formal or informal, who cares? The influence of public long-term care insurance. Health Econ. 2015;24:631–43.
OECD. Inflation (CPI) (indicator). OECD; 2022.
Kellerborg K, Brouwer W, Versteegh M, et al. Distributional consequences of including survivor costs in economic evaluations. Health Econ. 2021;30:2606–13.
University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Human Mortality Database. 2022.
Heijink R, van Baal P, Oppe M, et al. Decomposing cross-country differences in quality adjusted life expectancy: the impact of value sets. Popul Health Metr. 2011;9:17,7954-9–178017.
Attema AE, Brouwer WBF, Claxton K. Discounting in economic evaluations. Pharmacoeconomics. 2018;36:745–58.
Bonsang E. Does informal care from children to their elderly parents substitute for formal care in Europe? J Health Econ. 2009;28:143–54.
Gheorghe M, Hoefman RJ, Versteegh MM, et al. Estimating informal caregiving time from patient EQ-5D Data: the informal CARE Effect (iCARE) Tool. Pharmacoeconomics. 2019;37:93–103.
Hoefman RJ, van Exel J, Brouwer W. How to include informal care in economic evaluations. Pharmacoeconomics. 2013;31:1105–19.
Perry-Duxbury M, Asaria M, Lomas J, et al. Cured today, ill tomorrow: a method for including future unrelated medical costs in economic evaluation in England and Wales. Value Health. 2020;23:1027–33.
Brouwer WB, van Exel NJ, van Gorp B, et al. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006;15:1005–21.
Hoefman RJ, van Exel J, Brouwer WBF. Measuring care-related quality of life of caregivers for use in economic evaluations: CarerQol Tariffs for Australia, Germany, Sweden, UK, and US. Pharmacoeconomics. 2017;35:469–78.
Hoefman RJ, van Exel J, Rose JM, et al. A discrete choice experiment to obtain a tariff for valuing informal care situations measured with the CarerQol instrument. Med Decis Making. 2014;34:84–96.
Eurostat. Household composition statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Household_composition_statistics. Accessed 15 Dec 2022.
Acknowledgements
This paper uses data from SHARE Waves 1, 2, 4, 5, 6, 7 and 8 (DOIs: https://doi.org/10.6103/SHARE.w1.800, https://doi.org/10.6103/SHARE.w2.800, https://doi.org/10.6103/SHARE.w4.800, https://doi.org/10.6103/SHARE.w5.800, https://doi.org/10.6103/SHARE.w6.800, https://doi.org/10.6103/SHARE.w7.800, https://doi.org/10.6103/SHARE.w8.800, https://doi.org/10.6103/SHARE.w8ca.800), see Börsch-Supan et al. [27] for methodological details. The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782, SHARE-COVID19: GA N°101015924) and by DG Employment, Social Affairs and Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This project received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement #754936 (COMPAR–EU—COMPARing the effectiveness and cost-effectiveness of self-management interventions in four high priority chronic diseases in EUrope).
Conflicts of interest/competing interests
Saskia de Groot, Irene Santi, Pieter Bakx, Bram Wouterse and Pieter van Baal have no conflicts of interest that are directly or indirectly related to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
Data sharing is not applicable to this article as no datasets were generated during the current study.
Code availability
The code is available on reasonable request.
Author’s contributions
IS and SG analysed the data and took the lead in writing the manuscript. PB, BW and PvB contributed to the design, interpretation of the results and to the writing of the manuscript. PvB supervised the project. All authors approved the final submitted version of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
de Groot, S., Santi, I., Bakx, P. et al. Informal Care Costs According to Age and Proximity to Death to Support Cost-Effectiveness Analyses. PharmacoEconomics 41, 1137–1149 (2023). https://doi.org/10.1007/s40273-022-01233-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01233-8