W O M E N ' S
H E A LT H
W O M E N ' S H E A LT H
Cervical screening
Cervical screening
Urinary stress incontinence
Urinary stress incontinence


Ovarian cancer
Ovarian cancer



W O M E N ' S
H E A LT H
W O M E N ' S H E A LT H
Cervical screening
Cervical screening
Urinary stress incontinence
Urinary stress incontinence


Ovarian cancer
Ovarian cancer


International Women's Day (IWD) (March 8) is a global day celebrating the social, economic, cultural, and political achievements of women. The day also marks a call to action for accelerating women's equality. IWD has occurred for well over a century, with the first IWD gathering in 1911 supported by over a million people. In today’s world, IWD belongs to all groups collectively everywhere across the world. In 2022, gender inequality continues across all walks of life including healthcare. The theme of this year’s event is #BreakTheBias.
Research carried out by the British Heart Foundation reveals a surprising statistic that in the UK, coronary heart disease kills twice as many women as breast cancer. According to Harvard Medical School, within a year of a first heart attack, survival rates are lower in women than in men. Within five years following a heart attack, women experience more fatal outcomes; 47 per cent of the women may die, develop heart failure, or suffer from a stroke - compared with only 36 per cent of men who have suffered a first heart attack.
In September 2019, the Women's Health Taskforce was established by the Department of Health in order to improve women’s health outcomes and experiences of healthcare. The taskforce was also established to build on recent progress in women’s health, and following a recommendation from the Scoping Inquiry into the CervicalCheck Screening Programme that women’s health issues be given more consistent, expert and committed attention. Following an engagement with more than 1,000 individuals and organisations representing women across the country, the taskforce
identified four initial priorities within its action programme:
Improve gynaecological health;
Improve supports for menopause;
Improve physical activity;
Improve mental health among women and girls.
In September 2022, Minister for Health Stephen Donnelly announced the establishment of dedicated specialist menopause clinics across Ireland. These clinics will form a core part of a new ap–proach to menopause care for women and will be supported by enhanced community and primary care supports as well as the publication of targeted and trusted sources of information for women experiencing menopause.
The first phase saw the development of a dedicated specialist menopause clinic. We in the National Maternity Hospital, Holles Street in 2021. The clinic provides multidisciplinary care to women and is supported by GPs with a certified special interest in the area of menopause and clinical nurse/midwife specialists. In addition to seeing women who meet the clinical criteria for referral to the service, the team also provides advice and guidance to GPs in the community to support the effective management of menopausal symptoms for women closer to home within primary care. It is intended that the clinic will be supported by the development of additional regional clinics throughout 2022.
The development follows the advice of the Women’s Health Taskforce and ringfenced investment through the Women’s Health Fund. The Department of Health and the Taskforce's partners include the European Institute for Women’s Health, the
HSE including the National Women and Infants’ Health Programme, the National Women’s Council of Ireland, the Irish College of General Practitioners (ICGP), the Institute of Public Health, and the Department of Justice and Equality. They continue to listen to women and girls and work with them in the design and delivery of health and social care, to promote a coherent, holistic approach to improving health outcomes and experiences for women and girls.
While the development of menopause clinics regionally is to be welcomed, all healthcare professionals, managers, service planners, and funders should be aware of the negative outcomes from conditions other than menopause, such as cardiovascular disease and respiratory disease in women. Wishing all our readers a happy International Women’s Day!
Imagine a gender equal world. A world free of bias, stereotypes, and discrimination. A world that's diverse, equitable, and inclusive. A world where difference is valued and celebrated. Together we can forge women's equality. Collectively we can all #BreakTheBias
NiGP is now a fully independent publication and is no longer the official journal of the IGPNEA. If you are interested in writing an article for NiGP, please email priscilla@mindo.ie

NMBI UPDATE
An exclusive update article for NiGP from the NMBI about its plans for 2022
14
ASTHMA
OF CARE
16
EDITOR
Priscilla Lynch priscilla@mindo.ie
CONSULTING EDITOR
Ruth Morrow
SUB-EDITOR
Emer Keogh emer@greenx.ie
CREATIVE DIRECTOR
Laura Kenny laura@greenx.ie
ADVERTISEMENTS
Ruth Morrow explains what the HSE’s new End to End Model of Care for Asthma means for general practice
ASTHMA IN WOMEN
Ruth Morrow discusses the management of women who have asthma, including asthma during pregnancy and menopause
20
CATCH-UP VACCINATION FOR CHILDREN
Dr Tom Barrett, Senior Medical Officer, HSE National Immunisation Office, explains the official guidance on catch-up vaccinations for children
24
EDUCATION
Dr Sarah Harney, University of Limerick, discusses how studying for a Masters in Health Professions Education can elevate your professional development
25 INCONTINENCE
Prof Barry O'Reilly, Consultant Obstetrician and Urogynaecologist, Cork University Maternity Hospital, gives a short overview of how to treat urinary stress incontinence in women

26
OVARIAN CANCER
Theresa Lowry-Lehnen gives a comprehensive overview of the presentation, diagnosis, and treatment of ovarian cancer
31 CERVICAL SCREENING IN OVER-50S
This article from CervicalCheck explores the barriers to cervical
screening in over-50s and how smear sampletakers can help improve uptake
36 OPINION
GPN Clare Conlan gives a searing account of five minutes as a general practice nurse during the pandemic
37
COVID-19 AND GPN s
Priscilla Lynch reports on the anger of general practice nurses at being excluded from the pandemic bonus payment and being labelled as nonfrontline healthcare workers
39 OSTEOPOROSIS
Priscilla Lynch outlines how GPNs can support their patients with osteoporosis
42 BOOK REVIEW
Dr Karen Enright reviews a major new Irish textbook on dermatology in primary care
46 PRODUCT NEWS
A round-up of the latest pharmaceutical news
48 CROSSWORD
Test your word knowledge
Graham Cooke graham@greenx.ie
ADMINISTRATION
Daiva Maciunaite daiva@greenx.ie
Please email editorial enquiries to Priscilla Lynch priscilla@mindo.ie
Nursing in General Practice is produced by GreenCross Publishing Ltd (est. 2007).
© Copyright GreenCross Publishing Ltd. 2022
Please email publishing enquiries to Publisher and Director, Graham Cooke graham@greenx.ie
The contents of Nursing in General Practice are protected by copyright. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means – electronic, mechanical or photocopy recording or otherwise –whole or in part, in any form whatsoever for advertising or promotional purposes without the prior written permission of the editor or publishers.
The views expressed in Nursing in General Practice are not necessarily those of the publishers, editor or editorial advisory board. While the publishers, editor and editorial advisory board have taken every care with regard to accuracy of editorial and advertisement contributions, they cannot be held responsible for any errors or omissions contained.
30 30%
of infants experience symptoms of regurgitation1
For bottle-fed infants with frequent regurgitation
For bottle-fed infants frequent regurgitation
ESPGHAN RECOMMENDS
March 2018
a stepped-care approach...
a stepped-care
REVIEW
the feeding history.
TRIAL
the feed volumes by more frequent feeds an appropriate daily a thickened formula.
Clinically proven to reduce infant regurgitation episodes by


Aptamil Anti-Reflux formula for the dietary reflux and regurgitation
PHARMACY OUTLETS
30 30% al. Pediatrics 2003;111:e355-9.
symptoms of regurgitation1 www.eln.nutricia.co.uk
Clinically proven to reduce infant regurgitation episodes by 78%2
AVAILABLE IN RETAIL AND PHARMACY OUTLETS
References: 1. Vandenplas Y et al., J Pediatr Gastroenterol Nutr 2015; 61(5): 531–537. 2. Wenzl TG et al. Pediatrics 2003;111:e355-9.
* European Society for Pediatric Gastroenterology, References: 1. Vandenplas Y et al., J Pediatr Gastroenterol
IMPORTANT NOTICE: Aptamil Anti Reflux
It should only be used under medical supervision, should not be used in combination with antacids nutrition for infants from birth and as part
Ireland: www.aptamilhcp.ie
Northern Ireland: www.eln.nutricia.co.uk
Ireland: www.aptamilhcp.ie
FOR HEALTHCARE PROFESSIONAL USE ONLY.
July 2020
2
GreenCross Publishing’s official arrangement with the IGPNEA regarding Nursing in General Practice (NiGP) journal has come to an end. The journal is now a completely independent publication, similar to our other market-leading medical publications, Medical Independent, Update Journal, Irish Pharmacist, and OTC Update. After a productive 14 year partnership, we wish the IGPNEA great success and good fortune in their future communications endeavours.
We are very excited about our plans for NiGP, and have updated its design to reflect this new chapter. We are delighted that Ruth Morrow will remain as Consulting Editor and we will continue to have regular contributions from Theresa Lowry-Lehnen and many other leading practice nurses and medical writers. We will continue to publish CPD modules, clinical articles, and the latest nursing news stories and updates from all relevant stakeholders. The journal will
continue to be published six times a year, but with full editorial independence from now on, thus retaining its key elements while increasing its readership and relevance to all general practice nurses.
As an independent practice nursing journal, we can now make the printed version of the publication available to every practice nurse in the country and not just IGPNEA members as was previously the case.
There is no subscription cost to receive the journal at your work practice address. If you wish to receive the journal to your home address, however, we have to please ask you cover the postage supplement cost of €12 per year (€2 per issue).
Should you wish to receive your personal print copy of the journal, simply scan one of the QR codes on page 9.
We welcome feedback and ideas for new content. If you wish to make a comment or submit an article please email NiGP Editor Priscilla Lynch at priscilla@mindo.ie.
The Nursing and Midwifery Board of Ireland (NMBI) has expressed its heartfelt solidarity with nurses and midwives in Ukraine following the military invasion of the country by Russia.
NMBI says it is acutely aware of the immense challenges now faced by Ukrainian nurses and midwives due to the casualties caused by the war, missile strikes on medical facilities, and the displacement of hundreds of thousands of people – most of them women and children.
NMBI wishes it to be known that the organisation stands in solidarity with our colleagues in Ukraine who are now faced with tasks beyond the normal call of duty. “They remain in our thoughts at this time.”
The specialist Complex Menopause Clinic at the National Maternity Hospital (NMH), Dublin is now open and seeing patients. The service is dedicated to helping patients with serious medical conditions to manage their menopausal symptoms.
The clinic, supported by funding from the Department of Health and HSE's National Women and Infants Health Programme, is the first of four publicly funded specialist Menopause Clinics in Ireland and is staffed by GP menopause specialists, a full-time nurse specialist and an administrative team.
Appointments can only be offered to suitable patients via GP referral.
Mary Brosnan, Director of Midwifery and Nursing at the NMH said: “This is a great stride forward for women’s health. We are delighted to have this dedicated, specialist clinic at the NMH. As a woman, a midwife and nurse, I am acutely aware of how challenging the symptoms of menopause can be and of the lifechanging benefits evidence-based treatment can give."
Dr Deirdre Lundy, GP and specialist in women’s health and menopause,
said: “I am delighted to be leading the menopause specialist clinic in the NMH. Most patients, who are troubled by menopause symptoms, are able to receive advice and treatment in the community through their GP, practice nurse or family planning clinic. Unfortunately, patients with certain medical conditions including thrombosis, cardiovascular disease, cerebrovascular disease, hormonesensitive cancers, etc, are advised to be seen by a 'menopause specialist' to discuss management options – we are now that complex menopause service.”
Smoking remains one of the key causes of preventable morbidity and mortality in Ireland. To mark National No Smoking Day on March 2, the HSE reached out to healthcare professionals to remind them of its many free resources to help patients to quit smoking.
The HSE QUIT service provides personalised, free support by phone, email, SMS and live chat. Smokers can make an appointment with a local stop smoking advisor and have a consultation in person, over the phone or online, or they can call (free call) 1800 201 203 or visit www.QUIT.ie for stop smoking tips and resources, a free QUIT kit, and to create a QUIT plan.
Prepare to quit - take a moment to write down your reasons for quitting. Keep them close to hand or even stick them on your fridge as a reminder to stay strong. Set a QUIT date.
Change your routine and habits - do you normally have a cigarette with a coffee or tea? Then change your routine – have a cup of water instead or hold your cup in the other hand.
Keep check on cravings –your craving for nicotine will peak at three-to-five minutes and will pass if you deal with it. Have your heard of the 4Ds? 1. Delay at least three-tofive minutes and the urge will pass;
2. Drink a glass of water or fruit juice;
3. Distract yourself, move away from the situation; and 4. Deep breathe –breathe slowly and deeply.
Get by with a little help from your friends – supportive friends, family, and even work colleagues could make all the difference to you on your QUIT journey.
Help yourself QUIT by getting support from the HSE’s QUIT Team. The HSE’s quit smoking service is available to everyone and is free of charge. By using a support service like this you are twice as likely to succeed.
Find stop smoking clinics and other services near your practice at www2.hse. ie/quit-smoking/support-services/.
Peer-to-peer support is available on the QUIT Facebook page www.facebook. com/HSEQUIT or on Twitter at HSE QUIT @HSEQuitTeam #TheLastStop #QuitandWin.
The health consequences of smoking tobacco impact women more in low socio-economic status groups where they are more likely to smoke to cope with negative emotions and stressful situations. Socio Economic Disadvantage (SED) contributes to higher tobacco use among adult women, which affects subsequent generations through role modelling or by exposure to second-hand smoke.
Researchers from the Discipline of Public Health and Primary Care, School of Medicine at Trinity College Dublin, undertook a pilot programme in response to the need to find more effective ways to engage SED women smokers in smoking cessation services and to improve health equity. Their findings are published in the journal of Nicotine and Tobacco Research
The study assessed a pilot communitybased stop smoking programme, ‘We Can Quit (WCQ), specifically designed for women living in SED communities in Ireland. It was developed initially by the Irish Cancer Society (ICS) in collaboration with the National Women’s
Council of Ireland, the Institute of Public Health and the HSE. Uniquely, the programme is delivered by trained local lay women (community facilitators).
The key components of the WCQ programme are:
Group-based support once a week for 12 weeks, delivered by Community Facilitators (CFs): Lay trained women living/working in target areas.
Access to nicotine replacement therapy (NRT) - free of charge for all participants who wish to take it.
Individual one-to-one text support between sessions.
Dr Catherine Hayes, Associate Professor in Public Health/Specialist in Public Health Medicine, Trinity and senior author of the new study on WCQ, said: “We Can Quit is an effective way to engage heavily dependent women smokers who experience multiple stresses through disadvantage, by delivery of an outreach programme in their own communities in a way that is meaningful for them and that directly addresses their needs.
“Having a community-based structure in place will facilitate future assessment of cost-effectiveness in terms of smoking cessation and expansion and integration of the programme into the HSE, which is currently in progress. Removing cost as a barrier to using NRT for those who attend smoking cessation programmes is an important issue for government policy.”
The research paper: Peer-delivery of a gender-specific smoking cessation intervention for women living in disadvantaged communities in Ireland. We Can Quit2 (WCQ2)—A pilot cluster randomised controlled trial is available here: https://doi.org/10.1093/ ntr/ntab242.

Diabetes SMART is a free interactive online education platform available at www.diabeteseducation.ie developed by Diabetes Ireland with support from Novo Nordisk. This free interactive programme has been updated to meet increasing demand from people with type 2 diabetes who want to learn more about their condition and how to manage it effectively.
Due to the significant burden placed on general practice and the healthcare system over the last two years because of the Covid-19 pandemic, many people with type 2 diabetes have not had regular review appointments with their GP, GPN, or their diabetes team. Diabetes
SMART is a valuable resource that will give those diagnosed within the last two years especially the opportunity to educate themselves about their condition and how to manage it effectively and will also act as a refresher programme for the thousands of people who are living with type 2 diabetes for longer. It is also a good education tool for GPs, GPNs and other health professionals to promote to their patients.
The Diabetes SMART programme contains six interactive modules, covering topics that explain what diabetes is, understanding
the key medical information, such as blood glucose levels and managing illness, and provides lots of tips on healthy eating and getting active. The course can be completed whenever and wherever suits, can be paused and continued at any time, and is accessible via a laptop, tablet, or mobile phone.
The programme has been developed by diabetes healthcare professionals to support a busy lifestyle and participants can pause their interactive learning
at any stage of the journey and resume with ease. This resource will give people with type 2 diabetes the knowledge and accessible tools to learn how to manage their condition from the comfort of their own home and protect their future health.
Speaking about her type 2 diabetes journey, Deirdre McTeigue who has trialled the programme, said: “I really liked the visuals and the videos. As I’m newly diagnosed, I’m finding it all a bit daunting, I like that I
can go back and look at the diagrams/videos again. I also like that I can share the material with my husband and children so they can understand and better support me. Especially as it’s also online, I can share it with my family. I find that they are now more willing to come out walking with me and more encouraging with the diet. Having diabetes is restrictive, but I now know, very manageable, and we can’t say that about a lot of illnesses.”

The Minister for Health Stephen Donnelly has approved the 2022 National Service Plan for the HSE which aims to reduce waiting lists, build hospital and other service capacity, and continue to support the progress of important Sláintecare reforms.
The National Service Plan outlines the health and social care services that will be provided to the people of Ireland in 2022 within the allocated budget of €20.7bn.
Minister Donnelly said: “This is the largest financial allocation ever received by the health and social care services and it comes at a time when we are continuing to deliver reforms and improvements based on the recommendations of the Sláintecare report towards the delivery of universal healthcare.
“This National Service Plan for 2022 will improve outcomes for people who need to engage with our public health service, continue to see capacity increased, build on the reforms and improve timely access.
“The plan supports health objectives set out in the Programme for Government, bringing us closer to universal healthcare, sees a huge focus on the promotion of women’s health, and in the post-Covid-19 environment we also focus on supporting positive mental health and wellbeing amongst others.”
Mr Paul Reid, CEO of the HSE said: “There is now renewed hope that we are moving towards a more normal environment in which we can tackle waiting lists, change
and improve how we do many things, and build on innovations made during the pandemic. During 2022, we will work to identify practical means to deal with the huge task in front of us to provide badlyneeded services to people who have been waiting for a long time.”
The National Service Plan envisages that bed numbers within acute settings will significantly increase, including 1,146 additional acute beds by the end of 2022 (849 of which will be open by end-2021) and 19 additional critical care beds, to bring the total number of adult critical care beds to 340 by the end of 2022.
The funding for the Enhanced Community Care Programme will see completion of the roll-out of 96 Community Healthcare Networks (CHNs) and 30 community specialist teams for older persons, as well as the establishment of 30 community specialist teams for people living with chronic disease, reducing our dependence on a hospital-centric model of care.
Crisis resolution services in mental health will continue to develop, with the addition of three teams and cafes in place by year-end, providing 900 additional interventions as alternatives to acute inpatient care and emergency department presentations. The CAMHS telehealth hubs initiative will also progress, developing two further hubs in 2022 with an anticipated 200 new service users seen. And the new National Forensic Mental Health
Service will be opened in Portane with an initial 110 beds, increasing to 130 during 2022. Increased resourcing of specialist eating disorder teams will support an additional 660 new cases per year, and additional early intervention in psychosis teams will support an additional 335 service users.
A total of 120,000 additional hours of personal assistant supports, and 30,000 additional hours of home support will be delivered in disability services.
The HSE will also establish three additional specialist centre-based services to provide 4,032 respite nights to 90 children and will be transitioning 63 people (with disabilities) under the age of 65 from nursing homes to the community.
The maximum time an outpatient will have to wait to be assessed by a hospital consultant will be cut to 18 months by the end of the year.
The plan aims to have an additional 210,000 inpatient and day care procedures, and 20,000 colonoscopies, carried out in 2022 compared with last year’s Service Plan.
There is provision for an additional 1.8 million home support hours, an additional 40,000 mammograms, and more than 15,000 additional cervical screens.
The HSE aims to employ an additional 5,500-10,000 extra whole-time equivalent staff.
Diabetes Ireland is urging adults of all ages who have diabetes to ensure they have a full and proper foot assessment by a podiatrist or other appropriate healthcare professional.
Long-term high blood glucose levels may make feet susceptible to injury and infection. A person with diabetes is 22 times more likely to undergo a nontraumatic lower limb amputation than an individual without diabetes.
Latest data available, obtained by Roisin Shortall TD, shows that 608 people with diabetes underwent a lower limb amputation in 2020, accounting for 69 per
Continued on pg 10
Practice nurse required for mixed GMS/private GP practice in Carlow.
Role to include phlebotomy, cervical smears, vaccinations, childhood immunisations, chronic disease management, blood pressure and ECG monitoring, wound management, ante-natal (optional), etc.
Computer literacy essential. Practice uses Socrates management
Practice nurse sought for Bayview Medical, Killiney Shopping Centre, Killiney, Co Dublin. 8-24 hours/week, depending on your availability. Basic clinical skills and ability to work as part of a team essential. New medical
Part-time General Practice Nurse sought for Rathgar Medical Practice, Dublin 6. Competitive rates and flexible hours for the right candidate. Friendly working environment. Previous practice nurse skills desirable but not essential. Training can be provided. Position available immediately.
Interested applicants please contact osullym@yahoo.ie with your CV
Nurse wanted for GP clinic in Cork City. No previous practice nurse experience needed! 1-2.5 days per week (flexible). Phlebotomy skills essential. Any other skills a bonus! Small practice. Pleasant working atmosphere. Very supportive staff. Nice patient cohort.
Informal enquiries in privacy to Dr Pat Hill: 086 852 5856 or email: pathill11@gmail.com with a cover note and CV

To receive your personal copy of the journal six times a year, sign up by scanning the QR code below that suits you.


OPTION 1
Free journal subscription
Delivery to your work address.
No postage charge
OPTION 2
Free journal subscription


Delivery to your home address.
€12 postage charge
cent of the total procedures carried out in the year. There was a further 2,536 people with diabetes hospitalised requiring foot ulceration treatment, spending on average 14 days in hospital for treatment in 2020. Despite limited access to diabetes review appointments during the past two years, it seems from this data that diabetes-related amputations and diabetes foot ulceration inpatient numbers remain high year-on-year. New data available on www.diabetes.ie provides a county-by-county breakdown of both diabetes-related lower limb amputations and diabetes foot ulceration inpatient numbers over the period 2016-2020. In 2020, there were particularly high increases in Wexford and Louth in terms of the number of people with diabetes requiring inpatient diabetes foot ulceration treatment.
With such high numbers, Diabetes Ireland is urging people with diabetes to be proactive by booking a foot assessment, which will identify any problems and allow treatment to be undertaken early, thus preventing more serious problems from occurring. It recommends that people should examine their feet daily and be on the lookout for small cuts, changes in skin colour and temperature, red areas, and swelling. They also must check they have continuing sensation in their feet and be alert to signs such as prickly pain in the feet, numbness, and peculiar sensations such as a feeling of walking on cotton or of wearing tight socks. This is important as without a pain alarm system, injuries and poor fitting shoes may go unnoticed.
Diabetes Ireland now has over 5,000 clients attending their preventative footcare services in Dublin and Cork. These services were set up to provide people with access to a high-quality podiatry appointment service offering a full diabetic foot screen and assessment, foot and nail care treatment, and callus and corn removal where necessary. A footwear assessment is also carried out with professional shoe fitting where necessary. A choice of footwear (shoes and socks) is available at extremely competitive prices. To book an appointment, ring 01 842 8118 or 021 427 4229 or log onto www.diabetes.ie.
Further information is available free online at www.diabetes.ie/living-withdiabetes/living-with-type-2/managingdiabetes/footcare/.
Dr Harry Barry, GP practitioner and mental health advocate, will deliver the keynote lecture at the inaugural Vhi 360 Masterclass, which will take place virtually on Saturday, March 26 from 9.30am-1.30pm. The Vhi 360 Masterclass brings together Vhi Health and Wellbeing clinicians to share their knowledge, experience and expertise on recent advances in clinical practice in the areas of paediatrics, sexual health, infectious diseases, chronic disease management, musculoskeletal medicine, integrative medicine, and lifestyle health.
Open to GPs, general practice nurses (GPNs), hospital doctors and HSCPs, the Vhi 360 Masterclass is free to attend, and accredited for 3.5 external CPD credits and half day GMS study leave. The overall aim of the virtual Vhi 360 Masterclass is to support improvements to patient care in primary care settings.
Dr Barry’s keynote lecture will look at selfcare for clinicians, approaches to burn-out, managing low frustration tolerance and
improving empathy skills.
Dr Barry said: “We are living in an age of deep frustration, deep disappointment and deep anxiety. There are very few people who remain untouched by the pandemic and now we are looking at the hourly news reports of war and suffering, so unsurprisingly resilience reserves are depleted. In my lecture I hope to provide GPs with some tools for self-care so that the skills they bring to work every day – empathy, patience, tolerance – are nurtured and nourished.”
The other speakers and topics they are covering are:
Dr Ceppie Merry, National Clinical Lead, Integrative Medicine, Vhi Health and Wellbeing, Consultant Physician in Infectious Diseases, will look at how integrative medicine is being used to manage infectious diseases.
Dr Mou Soutana, Counselling Psychologist, Psychotherapist, and Vhi Integrative Health Coach, Vhi Health and Wellbeing, will focus on consultation skills, specifically around the topic of gender
identification and sexual orientation.
Dr Wilby Williamson, Clinical Director for Integrative and Lifestyle Health, Vhi Health and Wellbeing, Consultant Sports and Exercise Physician, will look at emerging trends in Ireland in complex chronic disease management and talk about approaches to prevention and management.
Dr Olivia Murphy, Senior Clinical Psychologist, Vhi Health and Wellbeing, will talk about the trauma informed perspective on child development.
Dr Manoj Parameshwar, Consultant Paediatrician, Vhi Health and Wellbeing, will talk about ADHD management using nonpharmacological interventions.
Dr Suzi Clarke, MSK Clinical Lead, Vhi Health and Wellbeing, Consultant Sports and Exercise Physician, will focus on an integrative approach to the management of musculoskeletal injury and pain.
Vhi 360 is a new model of healthcare in Ireland and the opening of Vhi 360 Health Centre Carrickmines represents the introduction of this new model.
The Minister for Health, Stephen Donnelly TD and the Minister of State with responsibility for Public Health, Well Being and National Drugs Strategy, Frank Feighan TD have welcomed the extension of funding for the Sláintecare Integration Fund projectChildhood Obesity Training in Primary Care into 2022.
One-in-four children in Ireland are living with overweight or obesity and 1.8 per cent of children have severe obesity. Children living with obesity have a higher risk of adult diseases, such as stroke, cardiovascular disease and about 11 different cancers. They also are at risk of other childhood health complications and illnesses. At present, most health professionals do not receive any specific training on childhood obesity.
Facilitating Integration of Childhood Obesity Services in Primary Care through Education was piloted from funding provided through the Sláintecare Integration Fund. Funding for the continuation of the project in 2022 is being provided by Healthy Ireland. The project aims to equip health professionals with knowledge, skills and confidence to help and support children who have obesity around the country.
The project is a collaboration between the School of Physiotherapy at RCSI University of Medicine and Health Sciences, the Child and Adolescent Obesity Service in Children’s Health Ireland at Temple Street, UCD, GP representatives, the Irish Coalition of People with Obesity, and the Association for the Study of Obesity on the island of Ireland.
Minister Donnelly said: “The delivery of this free, high-quality training allows health professionals to develop their knowledge and aims to improve access to care for children and
adolescents with obesity. By improving training, the project facilitates health professionals to provide children and families with a better patient experience, including less stigmatising attitudes from health professionals.”
Minister Feighan said: “The theme for World Obesity Day 2022 is ‘Everybody Needs to Act’, and through this training, we are empowering health professionals to act sensitively, but decisively, to ensure better health outcomes for children in their adult lives.”
The training project aims to build health professional engagement and experience, to enhance knowledge, to address perceived communication barriers and low confidence, and to establish a community of practice.
The project team initially aimed to provide training for 75 health professionals through 2020. However, the planned deliverables were exceeded with over 1,100 health professionals registered for training with over 750 hours of training completed to date.
The Nursing and Midwifery Board of Ireland (NMBI) is expanding and changing for 2022 with several new directors in place and additional staff being recruited in its Registration Department.

Experienced civil servant Sheila McClelland was appointed permanent CEO at the regulator in January after two years in an interim role when she led a modernisation and digitisation programme at the regulator.
Ms McClelland told NiGP that she’s delighted to be able to lead the organisation for the next five years.
“I am delighted to have been given the opportunity to lead an excellent team of highly-motivated and dedicated staff,” she says.
“We are fully aware of our obligations to protect the public and protect the integrity of our professions and it is with that in mind that NMBI will embark on our largest ever stakeholder engagement programme later this year.
“We will be planning our next Statement of Strategy to cover the three years from 2023 to 2025 and we will be seeking guidance and input from across healthcare and from across the public on what that strategy should contain.
“I am really pleased to have an experienced senior management team, which will assist me in that engagement process and in our ongoing programme of change in the time ahead.”
Under Ms McClelland’s leadership, a number of recent senior appointments and key initiatives at NMBI are aimed at continuing improvements at the regulator.
Experienced nursing practitioner
Carolyn Donohoe was appointed Director of Education, Policy, and Standards (Nursing) in the summer of 2021 after a 16-year high level career at St Vincent’s University Hospital, Dublin. There she held a number of roles including Peri-Operative Directorate Nurse Manager, Assistant Director of Nursing, Clinical Nurse Manager, and Critical Care Nurse.
“When I read the NMBI job description, I realised that I had the right background and mix of skills to bring a new clinical practice perspective to such a leading position for the profession,” says Carolyn.
“It was as if all the roles I had taken on previously had led me to this point. Nursing education is one of my passions and to combine that with quality improvement, strategy and leadership is a dream come
true. It’s a privilege to be trusted with the future standards of the nursing profession and I have always embraced a challenge, so when I got the chance, I jumped right in.”
Carolyn is passionate about continuous education, adding: “All practice needs to evolve and education is the strongest and safest tool we have in our arsenal to make sure we are doing right by our patients,” she says.
“Education helps us to see outside of our own back yard. The best way to bring practice forward is by using international evidence to support what we do. As a regulator, we ensure that the education programmes available at undergraduate and post-graduate level are in keeping with our two briefs, to protect the public and to protect the integrity of the nursing and midwifery professions.
“We are in a time of great change and the design and content of the education programmes need to move with the needs of the public and the professions. What we have learned from Covid-19 is that change is essential and agility is key to survival. I see the next 12 months as a time of great disruption, but that is exactly what we need to keep nursing and midwifery relevant and responsive in the current healthcare environment.”
Another new member of the senior management team at NMBI is Ray Healy who was appointed Director of Registration (interim) in December. Ray joined NMBI from the Department of Health where he was Safe Staffing Project Officer, having worked in nursing at St James’s Hospital, Dublin, in the NHS in Oxford, England, and in the Beacon and Hermitage hospitals in Dublin.
Maintaining the Register and adding more new registrants in the year ahead is Ray’s key focus. A recent recruitment drive is adding significantly to the number of NMBI registration staff to deal with the increasing number of applications to join the Register, particularly from outside the EU.
“We are working really hard to process all applications,” says Ray. “It is vital that NMBI remains vigilant in examining all the applications we receive to fulfil our remit in protecting the public and supporting the professions to provide care to the highest standards. At the same time though we are very aware that we need to add more registrants to fill the increasing number of posts required in all healthcare settings.
“Over the past few weeks, we have engaged with key stakeholders on this, and our goal is to assist applicants as much as possible from the outset to ensure they can progress through the registration process as efficiently as possible. It’s a busy department – in 2021 we issued almost 3,000 decision letters to those applying to join the NMBI Register. In all, 5,008 nurses and midwives were added to the Register last year.”
The NMBI is also working hard to improve its
Fitness to Practise function, led by Director Colm O’Leary, who took up the role in late 2020. Although fewer than 1 per cent of registered nurses and midwives will ever be involved in a Fitness to Practise complaint, Colm is aware that being the subject of a complaint can be a stressful and protracted process for a registrant and he is keen to ensure that complaints are brought to a conclusion as quickly as possible and is working hard on that.
Colm has been working in professional regulation for the past 17 years and was responsible for the establishment of the Register of Teachers in 2006. Before joining NMBI, he worked as Head of Registration with CORU.
Colm is using that breadth of experience to improve all aspects of Fitness to Practise in NMBI. In 2021, Fitness to Practise inquiries continued in remote and hybrid format allowing NMBI
to hold 64 inquiry days last year.
Colm says: “While my latest role is decidedly different to previous positions, which I have held at NMBI and other regulators, I am using those experiences to improve many aspects of the Fitness to Practise processes and to engage more frequently with stakeholders.”
In addition to rolling out a case management system within the depart–ment this year, he also intends to take steps to better inform those involved in Fitness to Practise processes.
This year NMBI will also be placing an increased focus on registrants and stakeholder engagement with the appointment of former Ministerial press advisor Kathyann Barrett as Head of Operations. Kathyann worked as advisor to the previous Minister for Health Simon Harris and has a background in corporate communications, politics, and journalism.
Kathyann says: “Working together with nurses and midwives, as well as other stakeholders in the health and education sectors, is at the heart of what we do in NMBI and is the best way to achieve our aim of enhancing patient safety and patient care. In 2022, we are committed to being more accessible to registrants and the public, as well as communicating more frequently and more effectively with all of our stakeholders.”
The new faces in the senior team join NMBI Director of Midwifery Dawn Johnson who celebrated five years in the role in February.
Dawn has had a 30-year career in midwifery in both the UK and Ireland and brings a wealth of experience and knowledge to her role.
Ms McClelland adds: “I am pleased to have such a dynamic senior leadership team who want to drive progressive change in the time ahead and engage more frequently with our registrants and stakeholders.

“We are listening to our registrants and learning from them all the time as we work together to advance nursing and midwifery excellence in Ireland.”
See www.nmbi.ie for more information.
WORKING TOGETHER WITH NURSES AND MIDWIVES, AS WELL AS OTHER STAKEHOLDERS IN THE HEALTH AND EDUCATION SECTORS, IS AT THE HEART OF WHAT WE DO IN NMBINMBI CEO Sheila McClelland AUTHOR: Ruth Morrow, Registered Advanced Nurse Practitioner (Primary Care); Respiratory Nurse Specialist (WhatsApp Messaging Service Asthma Society of Ireland); and Nurse Educator and Consultant

THE HSE’S NEW END TO END MODEL OF CARE DOCUMENT FOR ADULT ASTHMA OUTLINES THE STRUCTURES THAT HEALTHCARE PROFESSIONALS SHOULD ADHERE TO AND ADOPT IN THE CARE OF PATIENTS WITH, OR AT RISK OF, ASTHMA

Asthma is the most common chronic respiratory disease in Ireland, with approximately onein-10 of the population having asthma. Asthma control remains suboptimal in a large proportion of patients, which places significant health, social, and economic burden on the community and on healthcare. The reasons why asthma control remains poor is multi-factorial, but fragmented and unstructured care is believed to be an important contributory factor. The cost of asthma care in Ireland is over €500 million per annum, most of which is in secondary care.
The HSE’s new End to End Model of Care (MOC) for Asthma has been developed in consultation with a wide range of stakeholders including nurses, consultants, GPs, physiotherapists, patients, and patient support organisations. It covers the full spectrum of care provided in both hospital and in the community with a focus on developing partnerships between acute hospital services, general practice and community services, with the patient and his/her family being central to the model.
The End to End MOC for adult asthma
has been developed in tandem with the HSE strategy for chronic disease. It outlines the structures that we should adhere to and adopt in the care of patients with, or at risk of, asthma. This MOC is guided by national and international best practice.
The document is not meant to be a guideline document outlining interventions to be used in varied clinical circumstances that present when managing patients with asthma. In this regard the National Clinical Care Programme (NCP) Respiratory endorses the guidelines produced and updated regularly by the Irish Thoracic Society (ITS), the Irish College of General Practitioners (ICGP), and Global Initiative for Asthma (GINA). However, the MOC document details how patients should be able to access care at various stages of their asthma and also outlines the roles and responsibilities of the healthcare professionals (HCPs) providing this healthcare. It is envisaged that the implementation of this MOC will result in a reduction in the variation of care delivered to patients with asthma in Ireland and additionally result in an improvement in their asthma control, clinical outcomes and quality-of-life.
The MOC seeks, through the implementation of its guidelines, to improve the standard of care provided to adult asthma patients in all healthcare settings, with a particular focus on primary care where the majority of asthma is managed. This MOC will place a particular focus on the ‘at-risk’ patients who are vulnerable to developing asthma and those at risk of experiencing an acute asthma event. This includes those in lower socio-economic groups, smokers, patients with multiple co-morbidities, and those with psychological problems.
The MOC is a guide for best practice in the care of those at risk of developing asthma as well as those diagnosed with the condition across the continuum of care and includes both acute and chronic management of asthma in primary,
secondary, and tertiary care settings. The implementation of the MOC aims to ensure that optimum care is delivered using the principles of Sláintecare; so people with asthma receive the right care at the right time in the right place.
The spectrum of services, ranging from primary prevention to tertiary care, includes:
Primary prevention and health promotion.
Risk factor identification and management.
Early detection of asthma and its diagnosis.
Secondary prevention.
Primary care management of asthma.
Shared primary and secondary care management of asthma.
Secondary care management of chronic asthma.
Tertiary care.
The aims of the NCP for Respiratory specific to adult asthma are:
Maximise health and quality-of-life of people with asthma.
Minimise future risk for patients.
Prevent avoidable mortality due to asthma.
Standardisation of care for asthma patients in Ireland.
The objectives of the NCP for Respiratory include:
To improve access to structured integrated asthma care for patients diagnosed with asthma, which will address asthma education in the most appropriate setting.
To facilitate the provision of guideline concordant care, based upon a patient’s level of asthma control.
T o maximise the proportion of patients with asthma whose asthma is controlled.
To identify the appropriate resources needed to deliver on the aims of the NCP for Respiratory in relation to asthma.
In addition to guiding the delivery of the aforementioned objectives, this End to End MOC for adult asthma reflects the key reform themes identified by the HSE to improve the health of the population and to reshape where and how healthcare services are provided in Ireland. These themes include improving population health, delivering care closer to home, developing specialist hospital care networks, and improving quality, safety, and value.
The scope of this MOC is to define the services required to support the general population of adults in the management of their asthma. It includes health services operated and funded by the HSE and includes community-based services as well as access to hospitalbased secondary and tertiary care services if required. It acknowledges that specific health and social care settings, high-risk and vulnerable groups will require additional interventions and support. Working with other relevant national clinical programmes (paediatric and neonatal) and services, this MOC will inform the future development of shared pathways, policies, strategies and services to improve health outcomes in these settings. Supporting documents include clinical guidelines published by the ICGP, ie, Asthma - Diagnosis, Assessment, and Management in General Practice Quick Reference Guide. The National Clinical Guideline for the Management of an Acute Asthma Attack in Adults (NCEC) is also referred to in this document. International clinical guidelines, such as those from GINA (2021) underpin the diagnosis and management of asthma. Future development includes the NCP Respiratory collaborating with NCP Paediatrics and Neonatal to form a paediatric working group to develop Part 2: Paediatric Asthma.
Download the End to End MOC at: www.hse.ie/eng/about/who/cspd/ncps/ asthma/resources/end-to-end-model-ofcare-for-asthma.pdf for more information.
AUTHOR:

THIS ARTICLE EXPLORES THE CARE AND MANAGEMENT OF WOMEN WHO HAVE OR DEVELOP ASTHMA, INCLUDING ASTHMA DURING PREGNANCY AND MENOPAUSE, AS WELL AS ADDRESSING COMMON SITUATIONS WHICH WOMEN ENCOUNTER THROUGHOUT THEIR LIFETIME WHILST LIVING WITH ASTHMA
During childhood, boys have near twice the risk of developing asthma over girls. This changes once children reach the age of 12/13 years. Sex hormones, genetics, social and environmental factors, and responses to asthma treatments are important factors in the sex differences observed in asthma incidence, prevalence, and severity. In childhood, obesity, regardless of physical fitness, is associated with higher asthma prevalence and morbidity in girls, but not in boys. In girls older than 11 years and women, asthma is five-to-seven times more common in obese people compared to those of normal weight (Koper et al, 2017).
Asthma prevalence is higher in women who have multiple pregnancies, women whose periods started earlier in life and women with hormonal disturbances, such as polycystic ovarian syndrome
(Morales-Estrella et al, 2018). Women who are diagnosed with endometriosis also have an increased risk of asthma. A study by Morales-Estrella et al (2018) showed that 23.8 per cent of women who had endometriosis developed asthma, compared with 13.2 per cent of women who were taking oral contraceptives (OCS).
Testosterone, which increases in boys from the age of 12/13 years, has an anti-inflammatory effect in the airways and is thought to be one of the reasons why asthma is less prevalent in boys at this age. Female hormones increase at this age in girls, which is thought to increase the risk of developing asthma and increase symptoms in those who are already diagnosed with asthma.
As adults, women have an increased prevalence and severity of asthma. For women, fluctuations in sex hormone levels during puberty, the menstrual cycle, pregnancy, and menopause are associated with asthma (Nowrin et al, 2021). Later in
life, asthma incidence and severity are higher in women than in men, and highest in women between the fourth and sixth decade of life. During adulthood there is a shift to a female predominance, which affects mainly non-atopic asthma. In the elderly, the gender-related differences decrease. As testosterone levels decrease in older men, the incidence of asthma can also increase in this age group (Koper, 2017) In addition, pathophysiological abnormalities can be seen which includes blood eosinophilia, which seems to be more prominent in girls with asthma, but in adipose tissue. Girls with asthma tend to have a higher prevalence of non-eosinophilic asthma (60 per cent) compared to corresponding boys (30.8 per cent).
Severe asthma affects primarily boys before and at school entry age as well as women around the time of menopause. Women also develop ‘corticosteroidresistant’ or difficult-to-treat asthma more often than men (Moore et al, 2007). Studies show that compared to men, women can have worse symptoms more often:
Women are more at risk of acute asthma flare-ups and are admitted to hospital more often with their asthma.
Women who develop asthma for the first time later in life, after menopause, are more likely to have asthma that is difficult to control, and to need specialist care and treatments to help deal with their symptoms.
Lung function starts to decline after about the age of 35 years in both males and females. For women it declines more quickly after the menopause.
Statistics show that women with asthma over 65 years of age, are more at
Women can also have all the same triggers as men, but some of these triggers may be worse for women or affect them more often. For example:
Food allergies are more common in women than men with female hormones making them worse.
Cigarette smoke can affect women more than men. Women and girls may be more sensitive to cigarette smoke and girls with asthma who start to smoke may take longer and need more help to quit.
Stress, anxiety, and depression are more common in women, particularly older women who tend to be carers more often.
Indoor triggers, such as cleaning products, cooking fumes and house dust mites may affect women more as statistics show they’re more likely to be doing the cleaning at home.
risk of life-threatening asthma attacks.
Women who develop asthma at perimenopause tend to be less atopic, less corticosteroid responsive, and obese, with steroid refractory asthma (Moore et al, 2007, Wu et al, 2014). These women frequently require high doses of inhaled corticosteroids (ICS) to manage their asthma. Their asthma tends to be difficult to manage and have a higher rate of healthcare utilisation and poorer health outcomes.
Women are more likely to notice worse symptoms around times of hormonal change like puberty, menstruation, pregnancy, and peri-menopause. Not all women are affected.
One-third of women report worse asthma symptoms before or during a period.
Some women, particularly those with severe asthma, have worse symptoms during pregnancy. Although many women notice an improvement or no change at all when they’re pregnant.
Asthma symptoms can get worse during peri-menopause.
Women who have never had asthma can develop asthma at peri-menopause.
Hormones can be an asthma trigger in their own right, but they can also make the woman more sensitive to other triggers, such as hay fever or colds and flu. It is not yet clear why this is the case. It could be because it increases inflammation in the body and causes inflammation in the airways.
Having an annual asthma review including assessment of symptoms, checking adherence and inhaler technique and a review of their asthma ‘Action Plan’ can benefit women. At other times women should be advised that as they approach the peri-menopause, symptoms and asthma control may worsen and they should be advised to have an asthma review with adjustment of treatment if required. Risk can also be lowered by:
Taking the controller medicine every day as prescribed so that they are less likely to react to any asthma triggers, including hormones.
Keeping a symptom diary to help find out if hormones are triggering asthma symptoms around their menstrual period.
Keeping an eye on weight. Being obese increases the risk of asthma symptoms worsening as women get older. It also increases the risk of women getting asthma for the first time around menopause.
Discussing the woman’s risk of osteoporosis. Being on higher doses of inhaled steroids or needing regular or long-term courses of steroid tablets
WOMEN ARE MORE LIKELY TO NOTICE WORSE SYMPTOMS AROUND TIMES OF HORMONAL CHANGE LIKE PUBERTY, MENSTRUATION, PREGNANCY, AND PERI-MENOPAUSE
increases the risk of osteoporosis. Women are four times more at risk than men of developing osteoporosis. In women who have asthma, the chances of developing osteoporosis are slightly higher than average.
Being aware how other conditions could make asthma worse - for example, acid reflux, which is more common in women.
Around 20 per cent of women with asthma experience worsening of their asthma premenstrually. These women tend to be older and have more severe asthma, a higher BMI and have had asthma for a longer time (GINA, 2021). They also tend to have more menstrual abnormalities, such as dysmenorrhoea, shorter menstrual cycles, and longer menstrual bleeding. Paracetamol is usually safe, but non-steroidal antiinflammatory tablets (NSAIDs), such as ibuprofen (eg, Nurofen), and mefenamic acid (eg, Ponstan), and aspirin, may worsen asthma symptoms or trigger an asthma flare-up in some women. Oral contraceptives and leukotriene receptor antagonists may be helpful for these women.
Oral contraceptives (either the combined pill or the progestogen-only pill) are safe to take. Taking them at the same time as usual asthma medication will not affect the efficacy of either medication.
The morning-after pill, ellaOne, is not recommended for women with severe asthma. Some oral contraceptives are not recommended for women taking theophylline as plasma concentrations of theophylline are increased.
Data from 3,257 pre-menopausal Scottish women showed that hormonal contraceptives reduced asthma incidence and decreased asthmarelated healthcare utilisation, driven by a significant decrease in lean women, as well as decreased wheezing in asthma patients (Nwaru BI, Sheikh A, 2015). In a study by Morales-Estrella et al (2018), the prevalence of asthma was higher in women taking OCS than those who
weren’t (14.3 per cent vs 8.8 per cent). HRT also has asthma benefits and asthma risks:
Some research shows that HRT may increase the risk of women getting asthma for the first time.
Some studies show that HRT improves symptoms in women who already have asthma.
Generally, symptoms improve after the menopause, but this is not the case for women taking HRT.
Asthma control often changes during pregnancy – in approximately a third of women their asthma symptoms worsen, a third may improve, and the remaining third remain unchanged. Exacerbations are common in pregnancy, particularly in the third trimester. Uncontrolled asthma and exacerbations may be due to mechanical or hormonal changes or due to the stopping or reduction of medications due to concerns by the mother or healthcare provider. Pregnant women appear to be more susceptible to viral respiratory infections including influenza. Poor asthma control and exacerbations are associated with worse outcomes for the baby (low birth weight, pre-term weight, increased perinatal mortality) and the mother (preeclampsia). If asthma is well controlled during pregnancy, there is little or no increased risk of adverse maternal or foetal complications (GINA, 2021).
The advantages of actively treating asthma in pregnancy outweighs any potential risks from regular controller and reliever medications. Using medications to achieve good asthma control and prevent exacerbations is justified even if their safety in pregnancy has not been proven. The use of ICS, montelukast or theophylline is not associated with an increase of foetal abnormalities. There is plenty of evidence which shows that ICS reduce the risk of exacerbations during pregnancy and stopping ICS during pregnancy is a significant risk factor
for exacerbations. During labour and delivery, women should be advised to continue their usual controller medications and use their reliever if needed (GINA, 2021). Acute exacerbations are not common during labour, but bronchoconstriction may be induced by hyperventilation and should be managed using short-acting bronchodilators.
This article has reviewed the impact asthma has on women and provides some management strategies to help women cope with and manage their asthma, which can change throughout the lifecycle. Perimenstrual asthma, asthma in pregnancy, and asthma during the menopause have been explored with some useful management strategies to assist GPNs in providing care to women. ●
1. Global Initiative for Asthma. Global strategy for Asthma Management and Prevention, 2021. Available from www.ginasthma.org
2. Koper I, Hufnagl K, Ehmann R. Gender aspects and influence of hormones on bronchial asthma – secondary publication and update. World Allergy Organ J. 2017 Dec 27;10(1):46
3. Moore WC, Bleecker ER, CurranEverett D, et al. Characterisation of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Programme. J Allergy Clin Immunol 2007; 119: 405-413
4. Morales-Estrella JL, Zein JG. Oral contraception is associated with higher risk of lifetime asthma in women of reproductive age. Am J Respir Crit Care Med 2018. 197; A1342
5. Chowdhury NU, Guntur VP, Newcomb DC, Wechsler ME. Sex and gender in asthma. European Respiratory Review; 2021 30: 210067
6. Nwaru BI, Sheikh A. Hormonal contraceptives and asthma in women of reproductive age: analysis of data from serial national Scottish Health Surveys. J R Soc Med 2015; 108: 358-371




































































































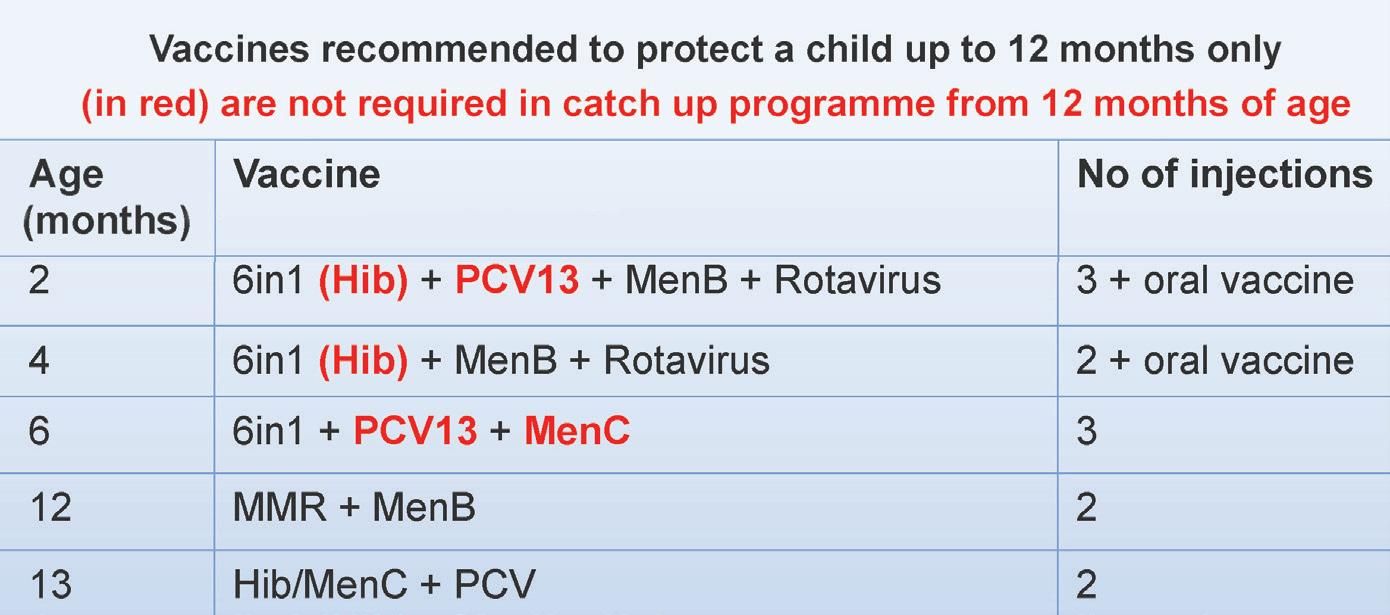
There has been a decline in the uptake of primary childhood immunisations in many countries in Europe including Ireland, particularly since the Covid-19 pandemic. Declines in immunisation coverage are a real concern, leaving young children vulnerable to vaccine preventable diseases, and leading to a risk of outbreaks. The HSE National immunisation Office has developed a toolkit to support GPs and general practice nurses to maximise uptake of childhood immunisations in your practice.
In Ireland the National Immunisation Advisory Committee (NIAC), an expert committee of the Royal College of Physicians of Ireland (RCPI), makes recommendations on vaccination policy.

The Department of Health is guided by NIAC recommendations. NIAC advises the vaccines included in the primary childhood immunisation programme are commenced at two months of age and are provided over five visits to protect children when they are most vulnerable to vaccinepreventable infectious diseases.
However, for various reasons children often present late for vaccination or may present from other jurisdictions having commenced a different vaccine schedule.
NIAC provides a catch-up vaccination schedule to facilitate vaccination of children (and adults) who present late for vaccination ( Table 1).
Since March 2020 the Immunisation Guidelines for Ireland from NIAC advise MenB vaccine catch-up is only recommended when a child reaches the age of two years if the child is in an at-risk group for meningococcal B disease. This is because the risk of meningococcal B disease is greatest in the first two years of life.
The Immunisation Guidelines also advise PCV13 vaccine catch-up is only recommended when a child reaches the age of two years if the child is in an at-risk group for pneumococcal disease.
Perhaps the most important point in the catch-up programme is that you never need to restart any of the recommended
vaccines’ schedules regardless of the time interval from the previous incomplete schedule. This is because of immunological memory.
Intervals longer than routinely recommended between doses do not impair the immunologic response to live and inactivated vaccines that require more than one dose to achieve primary immunity. Similarly, delayed administration of recommended booster doses does not adversely affect the antibody response to such doses.
This means that if a child has only had one 6-in-1 vaccine aged two months and the schedule is interrupted either until the child is aged one year or nine years, that child will always require 6-in-1 vaccine by two to complete the 6-in-1 vaccine schedule.
MenB 2 doses ≥8 weeks apart (if aged >10 months give 1 dose and a booster at >12 months ≥8 weeks after the first dose
8 months 0 days)
NOTE Continue with routine childhood immunisation schedule from 12 months
Routine school immunisations with Tdap/IPV >6 months and preferably 3 years after primary course and MMR2 >1 month after MMR1
Tdap/IPV as school immunisation at least 6 months and preferably 3 years after primary course and MMR2 >1 month after MMR1
Booster of Tdap/IPV 5 years after primary course; Tdap 10 years later
1. Hep B vaccine is not needed if this is the only vaccine required unless in a risk group (Chapter 9)
2. One dose of single Hib vaccine may be given to children from 12 months to <10 years of age if this is the only vaccine required
3. One dose if aged 7-<8 months
4. One dose if not yet in primary school and second dose will be given in junior infants
5. For HCWs or contacts in outbreaks born in Ireland since 1978 or born outside Ireland, and for adults from low resource countries, without evidence of two doses of MMR vaccine
6. Only one dose of Tdap/IPV is required due to likely previous exposure to pertussis infection
TABLE 1: Catch-up schedules for children and adults. (Source: http://bit.ly/NIACCh2)
The number of vaccine doses in a recommended schedule in childhood is dependent on:
1. The vaccine being given –During childhood diphtheria, tetanus, pertussis, polio, and hepatitis B vaccines all require three doses of each vaccine to complete primary immunisation.
2. The age the vaccine is being given –For other vaccines in the schedule the number of vaccines recommended depends on the age of the child when they start the catch-up programme.
If a child starts the catch-up schedule
before 12 months of age the child will be recommended three doses of Hib vaccine (given in 6-in-1), two doses of PCV13 vaccine, and one dose of MenC vaccine. The MenC, PCV13 by two and Hib by three (in 6-in-1) vaccines recommended before 12 months of age are given to protect a child to 12 months of age only.
A child starting vaccines between 12 months and <10 years still requires three doses of the diphtheria, tetanus, pertussis, polio, and hepatitis B vaccines. This means if a child attends after 12 months of age having missed their six-months vaccines visit, the child only requires the 6-in-1 vaccine missed at six months, which can be given with the MMR and MenB vaccine recommended at 12 months of age.
From the age of 12 months a child needs only one dose of PCV13 (to the age of two years), MenC (up to when MenACWY is offered), and Hib (up the age of 10 years) ( Table 3).
If a child is late attending for their six-months vaccines visit but is not yet 12 months of age there is no need to delay the 12-months vaccinations.
If a child attends later for their 12 months vaccines, they may be given their 12- and 13-months vaccines at the same time, if the parents are happy to receive this and particularly if there are concerns the parents may not return for the 13-months vaccines. These four vaccines are given together routinely in the UK.

MenB vaccine schedule also depends on age. If the child is aged 10 months or more, the child starting MenB vaccine schedule only need two doses of MenB vaccine. However, if the schedule was interrupted and the child received one dose of MenB vaccine at two months, that child still needs three doses of MenB vaccine to complete the schedule because the first dose was given before 10 months of age.
3 to <10 months*
3 2 doses 2 months apart. 3rd dose at ≥12 months
>2 months after dose 2
10 months to <2 years
2 years and older
2 2 months apart
2 1 month apart
*Bexsero® given at age 2 and 4 months (or up to 12 months) should be given with paracetemol, and in a different from the other childhood vaccines
The optimal recommended ages and intervals provide the best immune response.
The minimum interval is the shortest time between two doses of a vaccine in which an adequate response to the second dose can be expected.
The Immunisation Guidelines advise that in exceptional circumstances (eg imminent international travel, measles outbreak, and catch-up) it may be necessary to provide one or more vaccines at less than the optimal age or interval.
This accelerated schedule should not be used routinely. Remaining doses should be given at recommended intervals to ensure the best protection.
The minimum interval between dose one and two of MenB vaccine given before 10 months of age is four weeks. Therefore, in exceptional circumstances and before 10 months of age for MenB vaccine, you can give the second dose after four weeks rather than leaving an eight weeks interval in exceptional circumstances.
The minimum interval between dose one and two of rotavirus vaccine given before eight months of age is four weeks. Therefore, in exceptional circumstances and before eight months of age, you can give the second dose of rotavirus vaccine after four weeks rather than leaving an eight weeks interval.
If a child has received one or two doses of rotavirus vaccine in another country it is important to establish which rotavirus vaccine was given. The Immunisation Guidelines advise: “If any dose in the series was RV5 (Rotateq) or the vaccine product is unknown for any dose in the series, a total of three doses of rotavirus vaccine should be administered if the infant is at an age when the vaccine can still be given.”
If an infant presents later than 15 weeks of age and has not received rotavirus vaccine the infant can still receive the first dose up to the seven months and 0 days and receive the second dose before eight months and 0 days.
When hepatitis B (HepB) vaccine was added to the childhood immunisation schedule in 2008 there was no catch-up
programme for children in Ireland already vaccinated with 5-in-1 unless they were in an at-risk group. HepB vaccine catch-up is recommended onlyif a child is in an at-risk group.
The HepB vaccine is available from the National Cold Chain Service for children in at-risk groups only.
If a child has received MMR vaccine by two doses given at least four weeks apart from the age of 12 months, the child has completed the MMR schedule. Some countries now give the MMR vaccine at 12 and 18 months of age.
Remember that you never need to restart the schedule for any of the vaccines listed below:
6-in-1 x three doses, eight weeks apart;
MenB x two doses, eight weeks apart;
MMR, MenC, PCV13 x one dose;
6-in-1 x three doses, eight weeks apart;
MMR, MenC;
(MenB and PCV13 not recommended when a child reaches the age of two years);
If missed MMR + 4-in-1 in school;
Second MMR and DTaP/IPV (recommended six months after third 6-in-1 vaccine).
4-in-1 (Tdap/IPV) x three doses, one month apart + fourth dose in five years;
Low-dose diphtheria and pertussis vaccines are recommended for those aged 10 years;
MenC (MenACWY only given in second level schools).

Immunisation Guidelines: http://bit.ly/NIACGuideline
Useful link for accessing vaccine schedules in the EU: https://bit.ly/VaccScheduler
WHO link for accessing vaccine schedules worldwide: https://bit.ly/WHOSchedules
Toolkit for GP Practices to increase primary childhood vaccine uptake from HSE National Immunisation Office: https://bit.ly/PCIToolkit
1Children can be vaccinated with MMR between 6 and 12 months, eg, during a measles outbreak. If so, they should have a repeat MMR at 12 months of age, at least one month after the first vaccine, with a third dose at 4-5 years of age.
TABLE 5: Optimal and minimum recommended ages and intervals between doses of the Primary Childhood Vaccination Schedule. (Available at: http://bit.ly/NIACCh2)
Primary Immunisation Schedule Catch-up v accination presentation from Dr Tom Barrett, Senior Medical Officer, HSE National Immunisation Office: https://youtu.be/JpmWiSRY4So
The impact of the recent Covid-19 pandemic and the required changes in education have highlighted the priorities in delivering quality education in the health professions. The demands of delivering theory-based learning with practical skills training and workplace-based experiential learning forced rapid adaptations and drove many innovations in health professions curricula. With more time to now adapt and adjust to a new educational era, what do we take from this experience to optimise our educational systems?
As educators we need to adopt teaching strategies that enable flexibility, inclusivity, and contribute to excellence in academic outcomes and learner-centred experience. Such changes can be underpinned by understanding of educational theory and studying for a postgraduate qualification, such as a Masters in Health Professions Education (HPE), can be an inspiring introduction to developing an evidencebased, innovative teaching practice.
The Masters in HPE at the University of Limerick was developed for healthcare professionals who are interested in and/ or involved in delivering education and training at all levels. It attracts a diverse range of health professionals with current students and alumni from disciplines in nursing, medicine, allied health therapies, paramedicine and social care. Our students range from recent graduates with an interest in teaching to veteran educators with years of practical experience in clinical education.
The course is accredited by the Academy of Medical Educators (AOME), the organisation whose professional standards serve as a guide for excellence in curriculum development
in health professions education. This accreditation means that the M.Sc HPE programme has been externally validated and found to meet the AOME’s quality standards. For graduates of the programme, this award will automatically entitle them to membership of the AOME, to use the post-nominal letters MAcadMEd and demonstrates that they have been judged to meet the Academy’s Professional Standards for Medical Educators at an appropriate level.

Designed with recognition of the challenges of managing full-time work, often involving shifts and irregular hours, with part-time study, this course is offered in two formats: A fully-online, distance-learning format and a blended format. This flexible format means that course content is made available online at the beginning of each module so that learners can study asynchronously at their own pace while online sessions provide opportunities for interaction and collaboration with fellow students and academic faculty. In addition, interactive, workshop-style study days can be attended in person or online, and recordings are also made available online to access at other times. Collaborative activities enable learners to become part of an interprofessional community of practice with other educators.
How we learn and how educators can best promote and support learning are described by many theories and principles that span all disciplines. However, HPE is a complex area with learners required to gain theoretical knowledge and understanding combined with practical skills mastery and professional attitudes and behaviour. This requires quite a specialised set of teaching strategies, varied
formats and appropriate, valid assessments of learning. Supporting learners in the workplace and fostering their professional identity development is also a complex task and one that is often done alongside the demands of service provision. Modules tailored to these unique demands of HPE cover specialised aspects of assessment, educational support, leadership, and curriculum design in the health professions, all underpinned by educational theory. Following training in educational research methods, students complete a research project, supervised and supported by two members of academic faculty with extensive research experience. Students have scope to research a topic of interest in their own discipline and teaching practice. In addition to bringing about a better understanding or change in their own context, students can expect to publish their work in a peer-reviewed journal.
Most committed educators are motivated by an interest in teaching and are passionate about education and supporting their students’ learning and professional development. Having an educational qualification can give healthcare educators an edge in developing an effective teaching practice and can also be helpful for career progression with many schools and institutions favouring academic staff with formal educational qualifications. For your students and trainees, an informed and inventive approach to curriculum delivery can support improved engagement and academic outcomes.
If you are interested in this course and would like further information, see www.ul.ie/ medicine/msc-healthprofessionseducation or email enquiries to mschpe@ul.ie. Applications are currently being accepted for September 2022, closing date June 30.
One of the most common medical conditions that affects the bladder is urinary incontinence. This type of incontinence can affect both sexes, but it is most common in women. In fact, according to the American Academy of Physicians (AAP), almost 50 per cent of women in their 40s and 50s have some form of urinary incontinence. This may either be an overactive bladder or urinary stress incontinence.
Urinary stress incontinence is the uncontrolled loss of urine, which occurs when a physical movement or activity like running, lifting weights, coughing or just sneezing, increases the abdominal pressure, affecting the bladder. People may have urine leakage when coughing, sneezing or laughing. Also patients can have a urine loss while standing up, getting out of the car or having sex. Basically, any activity that increases the abdominal pressure can lead to urine loss, especially if the bladder is full.
It is very important to know that this type of incontinence is not related to psychological stress, but it can make people feel embarrassed, possibly placing limitations and changes in their work and social life.
The main cause of this condition is the weakening of the pelvic floor muscles, which are the ones that support the bladder, among other pelvic structures. A secondary cause of this type of incontinence is the weakening of the urinary sphincter, which is the muscle in charge of controlling the release of urine. When these muscles become weak, anything capable of increasing the pressure outside
the bladder can lead to a urine leakage. Basically, these muscles can lose their strength due to:
Childbirth: this is the most common cause of the weakening of the pelvic muscles in women. During labour, some nerves and tissues can get damaged, leading to urinary incontinence sometimes quite soon after childbirth or even many years after birth.
Chronic sneezing and coughing, obesity, smoking, drinking alcohol, and high-impact activities like weightlifting or running are included as other factors that can increase the possibilities to suffer from urinary stress incontinence.
To be sure someone suffers from urinary stress incontinence, some of the following tests will be carried out:
Urinary stress test: The patient will be asked to cough while standing to see if there is any urine leakage.
Pad test: Women have to use a sanitary pad, while men use a special pad during an entire day or just while they are exercising to see how much urine they lose.
Cystometry test: This test measures the pressure of the bladder and the urine flow. Urine analysis: This can show if there is something abnormal in the urine like bacteria, blood, protein, or sugar.
Neurological exam: Used when needed to see if there is any problem with the pelvic nerves that can generate incontinence.
There are many ways to treat this annoying condition, from simple bladder and pelvic muscles exercises to surgical procedures.
Just by doing simple lifestyle changes, such as losing some weight, avoiding caffeine, alcohol, and cigarettes, practising regular exercises, etc, the patient can reduce bladder pressure, improving their day-to-day life.
The most common exercises to improve urinary stress incontinence symptoms are the Kegel exercises, which help to strengthen the muscles of the pelvic floor. Patients can do them anywhere at any time, without being noticed. These consist of squeezing the muscles that stop the urine flow for some minutes, a few times a day. It is basically the contraction of the pelvic floor muscles.
IncontiLase is a non-invasive Er:YAG laser therapy for the treatment of mild and moderate stress urinary incontinence, based on non-ablative photothermal stimulation of collagen neogenesis, shrinking and tightening of vaginal mucosa tissue and collagen-rich endopelvic fascia, and subsequently giving greater support to the bladder.
Regarding surgical procedures, the tension-free vaginal tape (TVT) and the trans-obturator tape (TOT) are widely performed. The TVT consists of placing a synthetic mesh around the urethra of the patient, increasing the positive pressure around the structures that allow urine flow. The other procedure, the TOT, consists of placing a permanent tape under the urethra. The purpose is basically the same as the TVT. The success rates of the surgical procedures are between 82 and 96 per cent. While these treatments help to reduce the symptoms of urinary incontinence, they rarely completely cure them. However, after surgery, the patient will be able to have an almost normal life.
For more information see https://professorbarryoreilly.ie/


IRELAND HAS ONE OF THE HIGHEST RATES OF OVARIAN CANCER IN EUROPE WITH THE MAJORITY OF CASES DIAGNOSED AT STAGE III-IV
Ovarian cancer is one of the most common cancers in women and more than 400 women in Ireland are diagnosed with the disease annually.1,6 Four-outof-five cases are diagnosed in women over the age of 50 years.6 The lifetime risk of developing ovarian cancer is 1.4 per cent in a woman with ovaries. 8
Ovarian cancer is the fifth most frequent cause of death in women globally, and the leading cause of death in women diagnosed with gynaecological cancers. The World Ovarian Cancer Coalition 2018 stated that “in 2012 there were 239, 000 cases, and 152,000 deaths worldwide from ovarian cancer, with some 600,000 women living within five years of a diagnosis. It is estimated that by 2035, incidence will increase to 371,000 a year (55 per cent rise) and deaths will increase by 67 per cent to 254,000.” 3
Early detection offers the best chance of survival; however, most cases of ovarian cancer are diagnosed at an advanced stage, leading to poorer outcomes. 2 Approximately 75 per cent of cases are diagnosed at an advanced stage due to non-specific symptoms. 8
Ireland has one of the highest rates of ovarian cancer in Europe. Figures from the European Cancer Information System for 2018 estimated that in Ireland the incidence rate of ovarian cancer is 16.1
per 100,000, compared with an average of 11.8 across the EU. 9,13 The incidence of ovarian cancer in Ireland is projected to rise – by 2045 cases of ovarian cancer are projected to increase by between 67-to-80 per cent with proportionate increases in treatment rates. Assuming that the average age-standardised rates during 2011-2015 continue to apply (‘demographic’ projection), annual numbers of cases of ovarian cancer are
projected to increase from 407 in 2015 to 731 in 2045 (+80 per cent). 9,10,11,12
In Ireland the majority of ovarian cancer cases are diagnosed at stage III-IV.9 Ovarian cancer was ranked the fourth most common cause of cancer deaths among women in Ireland between 2013-2015, with an average of 269 deaths annually.
Ovarian cancer is also one of the costliest cancers for household production losses per death. A productivity loss
analysis carried out in an Irish context (Pearce et al, 2016) projected that by 2030, premature death will cost a value of €367,284 household production losses per ovarian cancer death. 9
Ovarian cancer mostly affects postmenopausal women, where increasing age is associated with an increased incidence, advanced stage of the disease, and lower reported survival rates. The strongest risk factor for ovarian cancer is a positive family history of breast or ovarian cancer, where a personal history of breast cancer augments the risk. 2
Other risk factors include a personal/ family history of endometrial, prostate or colon cancer; faulty inherited genes including BRCA1 and BRCA2; increasing age – over half of all ovarian cancers occur in women over the age of 65; unexplained infertility, nulliparity, early menarche, late menopause, no history of oral contraceptive pill usage, and prolonged use of fertility drugs, especially if a woman does not conceive.6,8 Several studies have shown an increased risk caused by smoking, especially the risk of mucinous epithelial tumours.4,5 Protective factors include previous pregnancies, breastfeeding, oral contraceptive use, IUD insertion, and tubal ligation.8
Ovarian neoplasms are a heterogeneous group of tumours classified according to morphological and clinical features. The main subgroups are epithelial tumours, sex cord-stromal tumours, germ cell tumours, miscellaneous, and metastatic tumours. Approximately 60 per cent of all ovarian tumours and up to 90 per cent of all primary ovarian malignancies are epithelial. Epithelial tumours can be further classified as serous, mucinous, endometrioid, carcinosarcoma, clear cell, transitional cell, mixed epithelial, and undifferentiated carcinomas. The four most common histological types of epithelial ovarian cancer are serous, endometrioid, clear cell, and mucinous tumour. 2
Ovarian cancer can be classified into two subtypes, type I or type II tumours, with the latter being a more fatal variant, thought to be caused by continuous ovarian cycles leading to inflammation and endometriosis.
Type I tumours includes low-grade serous, endometrioid, clear-cell, and mucinous carcinomas, with the rare subtypes being seromucinous and Brenner tumours. Type I tumours mostly arise from atypical proliferative tumours, and usually present at an early stage and are low-grade except for clear cell which is considered high grade. Their proliferative activity is usually low. They are diagnosed early and carry a good prognosis.
symptoms of ovarian cancer can be vague and non-specific and easily missed in the early stages. Symptoms often become apparent in the later stages – stage III or stage IV. Presenting symptoms can include a combination of abdominal fullness, bloating, nausea, abdominal distention, early satiety, fatigue, changes in bowel movements, urinary symptoms, back pain, dyspareunia, and weight loss. 2
Investigation is guided by a complete history of the presenting symptoms, a thorough physical examination and assessment for risk factors.
Type II tumours include high-grade serous carcinoma, carcinosarcoma, and undifferentiated carcinoma, which mainly originate from serous tubal intraepithelial carcinoma. Type II tumours, in comparison, are highgrade and almost always of advanced stage. They have high proliferative activity with rapid and aggressive progression and a high degree of chromosomal instability compared to type I, with the presence of p53 mutations in most cases. 2
Currently, there is no screening programme for ovarian cancer because there is no screening test that is accurate and reliable enough to detect ovarian cancer in the general population.6 Initial
Physical examination includes recto–vaginal examination on an empty bladder to look for pelvic and abdominal masses in clinical cases of high suspicion. In advanced cases, a palpable pelvic mass or ascites or diminished breath sounds due to the presence of pleural effusions can also be found. 2 In patients with a high degree of clinical suspicion, radiological imaging including transvaginal ultrasonography (TVUS) and/or abdominal and pelvic ultrasonography is carried out. This provides information on the size, location, and complexity of the ovarian mass. Further imaging with chest and abdomen pelvis CT scan, pelvic MRI, and/or PET scan can be required. 2 CA-125 levels are checked in adjunction with the imaging. CA-125 is elevated in most epithelial ovarian cancers overall, but only half of early-stage epithelial ovarian cancers. The specificity and positive predictive value is found to be higher in postmenopausal women than in premenopausal women. CA-125 levels can also be used to calculate the risk of malignancy index (RMI). 2 Increased CA-125 levels are also observed in other physiological or benign pathological conditions, such as endometriosis, pregnancy, ovarian cysts, inflammatory peritoneal diseases, therefore other biomarkers are currently being studied to improve specificity for ovarian
TYPE I TUMOURS INCLUDES LOWGRADE SEROUS, ENDOMETRIOID, CLEAR-CELL, AND MUCINOUS CARCINOMAS
cancer biomarkers.
Human epididymis protein 4 (HE4) is a new biomarker that is currently being evaluated. It is more sensitive for ovarian cancer and found in approximately 100 per cent of serous and endometrioid subtypes. 2
Differential diagnoses for ovarian cancer can include colon cancer; embryologic remnants; gastric adenocarcinoma; metastatic gastrointestinal carcinoma; ovarian torsion; peritoneal cyst; retroperitoneal mass; uterine fibroids; endometriosis; papillary adenocarcinoma; serous adenocarcinomas; undifferentiated adenocarcinomas; small-cell adenocarcinomas; and Brenner tumours.2
It is recommended that all patients with tubo-ovarian carcinoma be offered germline mutation testing appropriate to sub-type. Specifically, testing of all high-grade non-mucinous carcinoma for BRCA gene mutations is recommended. 9 All tubo-ovarian carcinoma patients with a genetic test, which shows either a pathogenic variant or a variant of uncertain significance should be offered post-test counselling. If the patient has a significant cancer family history, even if BRCA1/2 testing is normal, a referral to genetic services is advised. 9
The stage of a cancer determines its size and whether it has spread. The grade refers to how abnormal the cells look under a microscope, and how quickly the cancer is likely to grow and spread. The four main stages of ovarian cancer are stage 1, 2, 3, and 4 using the International Federation of Gynaecology and Obstetrics (FIGO) staging system.7
The FIGO staging system is a surgical staging system which does not incorporate the grade of the tumour.
Stage 1: The cancer is only found in the ovaries. It is divided into three groups:
Stage 1A – the cancer is completely inside one ovary.
Stage 1B – the cancer is completely inside both ovaries.
Stage 1C is divided in to three groups: Stage 1C1 – the cancer is in one or both ovaries and the ovary ruptures during surgery.
Stage 1C2 – the cancer is in one or both ovaries and the ovary ruptures before surgery or there is some cancer on the surface of an ovary.
Stage 1C3 – the cancer is in one or both ovaries and there are cancer cells in fluid taken from inside the abdomen during surgery.
Stage 2: This means the cancer has grown outside the ovary or ovaries, and is growing within the pelvis. There may also be cancer cells in the abdomen. It is divided into two groups: Stage 2A – the cancer has grown into the fallopian tubes or the womb.
Stage 2B – the cancer has grown into other tissues in the pelvis, for example, the bladder or rectum.
Stage 3: The cancer has spread outside the pelvis into the abdominal cavity or to lymph nodes. It is divided into three groups – 3A, 3B and 3C.
Stage 3A is divided into two groups: Stage 3A1 – cancer has spread to the lymph nodes in the back of the abdomen.
Stage 3A2 – cancer cells are found in tissue samples taken from peritoneum, and it might also be in the lymph nodes.
Stage 3B – means there are cancer growths 2cm or smaller in size in the peritoneum and there might also be cancer in the lymph nodes.
Stage 3C – means there are cancer growths larger than 2cm in size in the peritoneum and there might also be cancer in the lymph nodes.
Stage 4: The cancer has spread to other body organs, such as the liver or lungs. Stage 4a – means the cancer has caused a pleural effusion with positive cytology.
Stage 4b – means the cancer has spread to the inside of the liver or spleen; lymph nodes outside the abdomen; other organs such as the lungs. There is no single universally accepted system for grading ovarian cancers. Many studies have used different systems proposed either by the FIGO, the World Health Organisation (WHO), or the American Gynecologic Oncology Group (GOG).9 Grading refers to the cancer cells size and appearance under the microscope and how much they are like or unlike normal cells. They are graded 1 to 3.
Grade 1 or low grade (well differentiated): The cancer cells are very like normal cells in the ovary. They usually grow slowly and are less likely to spread.
Grade 2 or moderate grade (poorly differentiated): These cancer cells look less like normal ovarian cells.
Grade 3 or high grade: These cancer cells are very unlike normal ovarian cells. They usually grow quicker and are more likely to spread.14
Current recommendations are that serous carcinomas are graded as low and high grade; endometrioid and mucinous tumours are graded using the FIGO system for endometrioid carcinomas of the endometrium, and clear cell carcinomas, carcinosarcomas and un-differentiated carcinomas are considered by definition grade. 3,9
Treatment of ovarian cancer conventionally includes a combination of chemotherapy and surgery. The type of surgery depends on the stage of the cancer, and the FIGO staging system for ovarian cancer is applied to determine patient management and prognosis. The patient should be counselled about all the treatment options available along with prognosis at the time of diagnosis, depending on
the stage of presentation. 2 A holistic and empathetic approach for communications is required regarding disease prognosis and disease-related treatment choices, in addition to management of symptoms and psychosocial issues. All patients with ovarian cancer should have access to a gynaecology nurse specialist. 9
In the early stage of invasive epithelial ovarian carcinoma and if the cancer is only in one ovary, unilateral salpingooophorectomy while preserving the uterus and contralateral ovary may be carried out, with comprehensive surgical staging where lesions show a low likelihood of progressing to malignancy.
However, for advanced-stage ovarian cancer, a debulking surgery is carried out, comprising peritoneal washing, total hysterectomy and bilateral salpingooophorectomy (BSO), inspection of all abdominal organs and peritoneal
cent, while for women with large volume residual disease, the risk is estimated at 80-to-85 per cent.8 Patients with complete response are followed up for at least five years. Increasing CA-125 levels can be a symptom of recurrence, however, if not accompanied by clinical symptoms secondline treatment is not recommended.8
Debate continues whether neoadjuvant chemotherapy, which involves giving three cycles of chemotherapy prior to surgery and interval debulking surgery, may be superior to massive primary debulking surgery in advanced ovarian cancer.8
Intraperitoneal chemotherapy (where cisplatin and paclitaxel are injected into the abdominal cavity through a catheter) may be an option in select patients, but controversy remains about its usage and benefit.16
Although there is a high response rate to initial treatment, the majority of
be used to help relieve symptoms in patients with more advanced disease. The treatment may be as short as one session or continue for several weeks, depending on the stage of ovarian cancer.1,2
Targeted therapies, eg, bevacizumab, a monoclonal antibody directed at vascular endothelial growth factor (VEGF), may be given along with chemotherapy, and it has been proven to be useful as maintenance therapy.1,14
PARP inhibitors are used to treat some women with advanced ovarian cancer that has returned after earlier treatment; eg, olaparib, niraparib and rucaparib in platinum-sensitive recurrent ovarian cancer.16 Results from clinical trials show that these drugs might also benefit women who are newly diagnosed with advanced ovarian cancer.15 Side-effects can be an issue in PARP inhibitors and must be carefully monitored for and assessed against quality-of-life. Nausea, vomiting, fatigue, anaemia, diarrhoea and arthralgia, and neutropaenia can all be observed across the PARP inhibitors, and niraparib also has thrombocytopaenia as a potential side-effect.16
surfaces, sampling suspicious areas for biopsy, total omentectomy and paraaortic lymphadenectomy.1,2,8 Primary debulking surgery consists of complete macroscopic tumour removal which could involve splenectomy, diaphragmatic resection, liver, intestinal or any other abdominal resection required to achieve complete cytoreduction. 8
First-line chemotherapy involves intravenous platinum/taxane regimes, carried out every three weeks for six cycles. For patients with FIGO stage 1A/1B and grade 1 and 2 tumours no further treatment is usually required.
Outcome is assessed by imaging results, usually CT scan, after completion of first-line chemotherapy.8 For women with residual disease of <1cm the risk of recurrence is estimated at 60-to-70 per
patients will develop recurrence. 8 About 80 per cent of women with advancedstage ovarian cancer more commonly have tumour progression or recurrence. Platinum free interval (PFI) is one of the most reliable predictors indicating the response of recurrent ovarian cancer to subsequent chemotherapy. PFI refers to the interval between the completion of the last platinum-based chemotherapy and the occurrence of relapse. However, platinum sensitivity is generally used to refer to an interval of greater than six months between the last platinumbased chemotherapy (PBC) cycle and commencement of subsequent PBC. 2
Radiotherapy is not a common treatment for ovarian cancer, although it may be used with chemotherapy and surgery to treat cancer. It can also
Immunotherapy, also called checkpoint inhibitor immunotherapy, in ovarian cancer is being studied in advanced disease with varied results. However, there have been no practisechanging trials so far.16
The prognosis of ovarian cancer is directly dependent on the disease stage at the time of diagnosis. It is also associated with baseline performance status, FIGO stage, and volume of residual disease post-primary cytoreductive surgery. The median survival of ovarian cancer patients is approximately 40-to-50 per cent at 10 years, with stage-related survival for stage 1 between 70-to-92 per cent compared to stage IV being less than 6 per cent. 2 In women with cancer that has spread to adjacent tissues, five-year survival rates drop to 80 per cent, and 25 per cent for those with metastatic
PARP INHIBITORS ARE USED TO TREAT SOME WOMEN WITH ADVANCED OVARIAN CANCER THAT HAS RETURNED AFTER EARLIER TREATMENT
disease. Patients with recurrent disease can be treated, however, they are usually incurable. Recurrent platinumsensitive ovarian cancer median survival is approximately three years; however, survival is approximately one year for platinum-resistant patients. 2
Ovarian cancer remains one of the most lethal malignancies in women, despite ongoing clinical trials and the introduction of new treatments in the past few decades. The poor clinical outcomes to date are mainly due to the failure of effective strategies for the early detection of ovarian cancer, chemotherapy resistance, and increased heterogeneity of the disease. With the goal for ovarian cancer to be diagnosed at an earlier and more curable stage, we are still in need of the development of effective strategies. 2
New agents are mainly directed against molecular target cancer cells proliferation pathways, tumour growth and escape from immune surveillance and death signals. These agents include anti-angiogenic factors, inhibitors of growth factor signalling, PARP inhibitors or folate receptor inhibitors. While not shown to be curative, these new agents are a step forward and may lead to the delay of recurrence or stabilisation of the illness. 8 Targeted therapy is one of the fastest growing modalities for cancer treatment. The use of targeted therapies has extended progression-free survival, but there is more work to be done and research and clinical trials are ongoing.
Vaccines are currently being studied for ovarian cancer, where the basis lies in activating the immune cells to destroy the cancer cells. The potential tumourassociated antigen molecules targeted in ovarian cancer in ongoing ovarian cancer vaccine research are CA-125, p53 protein, and HER2, among others. There are ongoing pilot and phase 1 or 2 trials for the use of therapeutic vaccines in ovarian cancer patients employing novel techniques. Other emerging therapies
1. Irish Cancer Society (2021). Ovarian cancer. Available at: www.cancer.ie/cancerinformation-and-support/cancer-types/ ovarian-cancer
2. Arora T, Mullangi S (2021). Ovarian cancer. StatPearls. Available at: www. statpearls.com/ArticleLibrary/viewarticle/95586
3. The World Ovarian Cancer Coalition (2018). The Every Woman Study. The world ovarian cancer coalition atlas: Global trends in incidence, mortality, and survival. Available at: https://worldovariancancercoalition.org/wp-content/uploads/2018/10/THE-WORLD-OVARIANCANCER-COALITION-ATLAS-2018.pdf
4. Torre L, Trabert B, DeSantis C, Miller K, Samimi G, Runowicz C, et al (2018). Ovarian cancer statistics, 2018. CA: Cancer J Clin 2018 Jul;68(4):284-296. doi: 10.3322/caac.21456
5. Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H. Ovarian cancer in the world: Epidemiology and risk factors. Int J Women’s Health. 2019 Apr 30;11:287-299. doi: 10.2147/IJWH.S197604
6. Marie Keating Foundation (2021). Ovarian cancer. Available at: www. mariekeating.ie/cancer-information/ ovarian-cancer/
7. Cancer Research UK (2021). Ovarian cancer: Stages and grading. Available at: www.cancerresearchuk.org/about-cancer/ ovarian-cancer/stages-grades
8. Javaid A, Kamran W. (2021). Ovarian Cancer a silent killer. Hospital Professional News. Issue 89; pp 57-57; October 2021
9. Department of Health (2019). Diagno-
being studied in clinical trials are using adoptive T-cell transfer and chimeric antigen receptor therapy (CAR-T) as a part of future strategies to ensure reduced cancer burden and improve life expectancy in this patient population. 2 Immune and cellular therapies coupled with genetic testing and precision assays (biomarkers) are promising strategies for better clinical outcomes. Novel strategies and research in this field will lead to better approaches to minimise ill health and improve life expectancy for patients with ovarian cancer.
sis and staging of patients with ovarian cancer: National Clinical Guideline No
20. Available at: www.hse.ie/eng/services/list/5/cancer/profinfo/guidelines/ diagnosis-and-staging-of-patients-withovarian-cancer.pdf
10. National Cancer Registry Ireland (NCRI) (2018a). Cancer factsheet: Ovary. NCRI, Cork, Ireland. Available at: www.ncri.ie
11. National Cancer Registry Ireland (NCRI) (2018b). Cancer in Ireland 19942016 with estimates for 2016-2018: Annual Report of the National Cancer Registry. NCRI, Cork, Ireland. Available at: www.ncri.ie
12. National Cancer Registry Ireland (NCRI) (2019). Cancer incidence projections for Ireland 2020-2045. NCRI, Cork, Ireland. Available at: www.ncri.ie
13. European Cancer Information System (2018). Available at: https://ecis.jrc. ec.europa.eu
14. Irish Cancer Society (nd). Cancer of the ovary: Caring for people with cancer. Available at: www.cancer.ie/sites/default/ files/2019-10/ovary_2015_web.pdf
15. NIH National Cancer Institute (2019). PARP inhibitors show promise as initial treatment for ovarian cancer. Available at: www.cancer.gov/news-events/cancer-currents-blog/2019/parp-inhibitors-ovariancancer-initial-treatment
16. Chauhan P, Westrup J. Updates in the management of ovarian cancer. Medical Independent. 2022 January 10. Available at: www.medicalindependent.ie/updatesin-the-management-of-ovarian-cancer/
VACCINES ARE CURRENTLY BEING STUDIED FOR OVARIAN CANCER, WHERE THE BASIS LIES IN ACTIVATING THE IMMUNE CELLS TO DESTROY THE CANCER CELLS
CervicalCheck offers free cervical screening to women and people with a cervix aged 25-to-65 years. The upper age limit changed from 60 to 65 years in April 2020 in line with the recommendations of the HIQA Health Technology Assessment carried out in 2017. This ensured that women who had turned 50 when the screening programme first began in 2008 would be eligible for at least one HPV test before exiting the programme. However, recent research carried out by the National Screening Service revealed that women aged over 50 have the lowest screening uptake, with one-in-four women in this age group not attending for screening.
The purpose of cancer screening is to detect pre-cancer or early-stage cancer in asymptomatic individuals, so that timely diagnosis and early treatment can be offered. Ireland has four quality-assured, organised, populationbased screening programmes under the management of the National Screening Service - BreastCheck, CervicalCheck, BowelScreen, and Diabetic RetinaScreen. Since the
introduction of CervicalCheck, the incidence of cervical cancer and its mortality rate has declined during the period 1994-2018. Cervical screening can save lives, decrease morbidity, improve quality-of-life, and deliver reassurance to individuals about their health.
The vast majority of cervical cancers are caused by the human papillomavirus (HPV). This aetiology provides an opportunity for the global elimination of this disease, which disproportionately affects young under-educated women in low- to middle-income (LMI) countries. In fact, the death rate from cervical

Over 6,500 women need hospital treatment for pre-cancer of the cervix (CIN)
Approximately 300 women are diagnosed with cervical cancer
Approximately 90 women die from cervical cancer
cancer is three times higher in LMI countries than in high-income countries like Ireland. Genital HPV is easily spread through sexual skin-to-skin contact. Infections are very common, with the incidence peaking between 18 and 30 years of age. There are 14 high-risk types of HPV, with types 16 and 18 causing over 70 per cent of cervical cancers. About 80 per cent of sexually active adults have been infected with one or more genital HPV strains at one time or another, but are unaware of the infection because HPV is usually spontaneously cleared by the body’s immune system. It is estimated that more than 90 per cent of women clear the infection spontaneously. However, a small percentage of women do not clear the infection and it can remain dormant or persistent, sometimes for many years.
There are two main types of cervical cancer; squamous cell carcinoma (77 per cent of cases) and adenocarcinoma (18 per cent). The remaining 5 per cent of cervical cancers are due to rarer histological types. It is now recognised that persistent HPV infection causes at least 92 per cent of cervical cancer in total and is responsible for 99 per cent of squamous cell cancers. Therefore, cervical screening with HPV and reflex cytology is more effective at reducing the risk of squamous
cell carcinoma than other histological cancer types. Adenocarcinoma of the cervix is a more aggressive type of cancer associated with a poorer prognosis. Cervical screening programmes internationally have had less impact on reducing adenocarcinoma than squamous cell carcinoma as adenocarcinoma cells typically develop within the endocervical canal, which may not be able to be sampled during the screening test.
Cervical cancer is preventable and curable, as long as it is detected early and managed effectively. There are two approaches to preventing cervical cancer: Primary prevention through HPV vaccination, and secondary prevention through effective screening and treatment programmes.
HPV testing was introduced as the primary cervical screening test in Ireland in March 2020. This is in keeping with other high-income countries such as Australia, Italy, the Netherlands, New Zealand, Sweden, and the UK. In 2017 a Cochrane review of 40 studies concluded that if 20 women out of 1,000 had precancerous changes, primary HPV screening would correctly identify 18 of these women, whereas primary cytology screening would only identify 15 of these women. HPV as a primary screening test, followed by reflex cytology in those that screen positive, will detect 90 per cent of women at risk of cervical cancer. This is significantly better than testing with a cytology-first test, which detects 75 per cent of women at risk.

CervicalCheck maintains a register of eligible women, calls and recalls them at predetermined intervals, and works with affiliate laboratories and colposcopy units to deliver the appropriate results and management recommendation for each screening
test. It is important to understand that the overall clinical governance for each woman remains with the clinicians involved, either in primary care or colposcopy. Collaboration between the administrative call-recall team, primary care sampletakers, cytology laboratories, colposcopy clinics, and histology laboratories is essential in order to provide a quality-assured screening programme.
In primary care, over 65 per cent of
cervical screening samples are taken by practice nurses. Sampletakers have a powerful role in making the cervical screening programme a success. Research shows that GPs and general practice nurses (GPNs) remain the most trusted source of information for most women. The relationship that develops between a woman and her primary care clinician can make the screening process clearer and less overwhelming, and ultimately increase
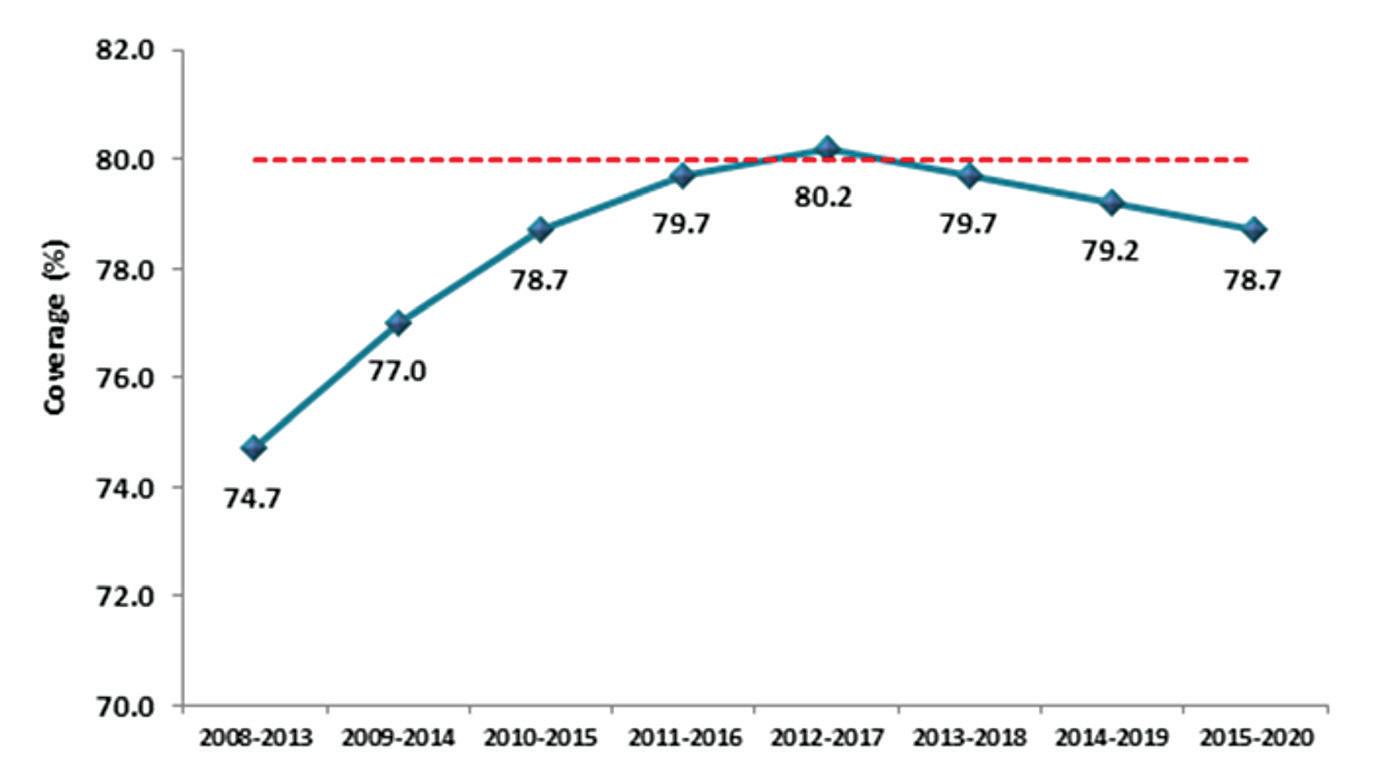
the participation of more women. GPs and GPNs are particularly well placed to reach out to under-served communities where screening rates can be low and incidence rates high, resulting in increased health inequities.
Screening coverage is defined as the proportion of individuals of the eligible population screened that has engaged in screening within a specific period, and directly correlates to the effectiveness of a screening programme. In keeping with the principles of screening, all screening programmes need to achieve high target coverage to be effective. CervicalCheck’s objective is to achieve at least 80 per cent population coverage during a five-year period. Figure 3 shows the five-year rolling averages since 2008, with a peak of 80 per cent in 2012-2017. Due to Covid-19 restrictions and public health advice, CervicalCheck paused cervical screening in primary care from March
to July in 2020. This led to a decrease in the number of women screened in 2020, but despite Covid-19 still being prevalent in our country in 2021, cervical screening testing in primary
has fallen to a 20-year low at just 70 per cent and coverage in the Netherlands is just 57 per cent.
care exceeded projected targets by 14 per cent. Population coverage for cervical screening in Ireland compares favourably with adjacent countries. In England, cervical screening coverage
Figure 4 shows the five-year coverage of eligible women by age group on the cervical screening register in Ireland and highlights that the 80 per cent standard for coverage was met in four of the eight five-year age bands. Consistently over the period of this report, younger participants (aged 25-to-29 years) have the highest coverage. It is worth noting that England, Australia, Canada, Sweden, Norway, France, and Italy have all documented that young women, particularly 25-to-30-year-olds, are the poorest attendees. Conversely, in Ireland, coverage is lowest in the 60+ age group, at just 60 per cent. In March 2020, CervicalCheck increased the age limit from 60 to 65 years alongside the change to a primary HPV programme. This unfortunately coincided with the arrival of the Covid-19 pandemic and those in the older age groups in society were advised to restrict their movements
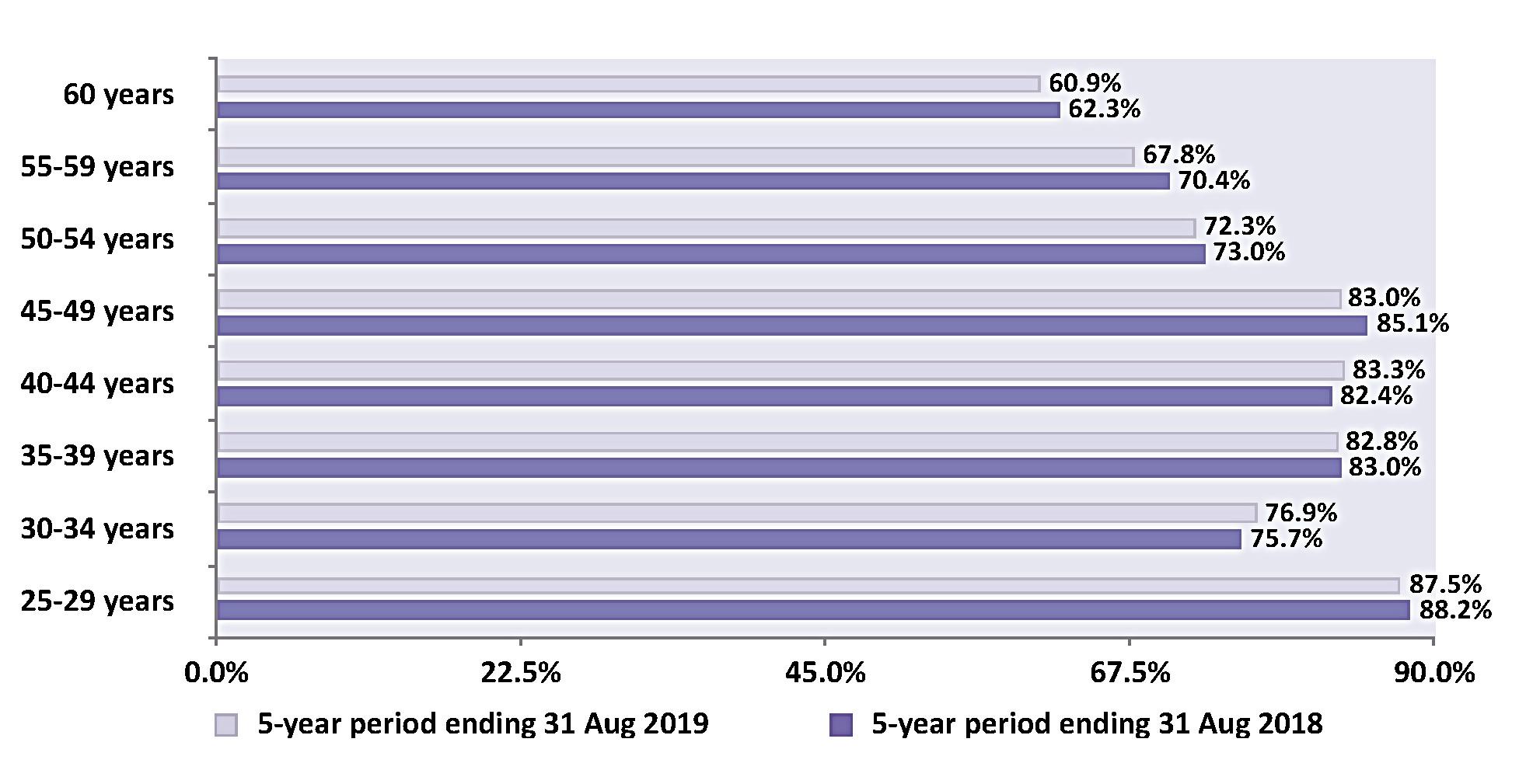
DESPITE COVID-19 STILL BEING PREVALENT IN OUR COUNTRY IN 2021, CERVICAL SCREENING TESTING IN PRIMARY CARE EXCEEDED PROJECTED TARGETS BY 14 PER CENT
for many months, meaning very few of those women would have attended for screening until absolutely sure it was safe to do so.
For women in the pre-HPV vaccine cohort (ie, those born before 1997 in Ireland), participation in cervical screening is their predominant means of preventing cervical cancer. Inadequate screening participation at age 50-to-64 years has been identified as a significant risk factor for cervical cancer for women in their 60s and 70s in a populationbased case control study examining the risk of developing cervical cancer in women aged 65-to-83 years. The study concluded that women are six times
more likely to develop cervical cancer if not screened between the ages of 50 and 64. If adequately screened, screening protection was greatest from 65-to69 years and decreased progressively since their last normal cytology test. Therefore, it is extremely important that women over 50 years engage with the cervical screening programme, as this will reduce their risk of developing cervical cancer and its associated mortality and morbidity in later life.
Numerous research studies have reported that women over 50 have multiple barriers to attending cervical screening. Overall, knowledge about both screening and HPV infection was
poor. Women associated HPV with sexual transmission, which caused feelings of embarrassment and unease with their own bodies and their sexuality. Fear that something was wrong was also identified as a deterrent towards screening. Pain and embarrassment during the procedure were noted at higher levels in older women. A recent survey conducted on behalf of the HSE stated women were also concerned about attending their screening appointment due to Covid-19.
Give information tailored to the needs of women over 50:
Figure 5 ‘Having the conversation’ highlights the information that women need to make an informed choice about participating in cervical screening. It is important to use open language and normalise HPV’s relationship to sexual activity. You can remind the woman that HPV can be picked up through any kind of sexual contact with anyone, even if the sexually activity was years ago.
Highlight the purpose of cervical screening: differentiate between screening and diagnostic tests.
Emphasise benefits of screening: screening saves lives, it identifies HPV before it causes cancer and helps identify abnormal cell changes when they are easier to treat.
Explain limitations of screening: it does not prevent all cases of cervical cancer, as cervical cancer can develop in between screening tests which is why symptoms should never be ignored.
Explain the risk factors for cervical cancer: smoking, early age at first intercourse, persistent HPV infection.
Normalise HPV infection by making women aware that even being with one partner means that they still have an 80 per cent chance of contracting HPV infection, and emphasise the ability of HPV infection to lie dormant for many years (this means that previous screening tests
may have been normal).
Reassure that most people's immune system clears HPV from their body within 18 months without any treatment. For some people the infection remains and this is why a repeat test in 12 months will check if the infection has gone.
Explain that in the absence of persistent HPV, it is safe to repeat the next screening test in five years. Without HPV infection, abnormal cells typically return to normal without intervention.
Explain that if testing detects persistent HPV infection, referral to colposcopy is initiated. This does not mean that you have cancer but means the colposcopy procedure will identify abnormal cell changes when it is easier to treat.
Emphasise that regular screening between age 25 and 65 years has a protective effect even after a woman completes cervical screening.
Actively encourage participation in screening:
Sampletakers need to actively remind women to use the ‘check the register’ function on the CervicalCheck website. Sampletakers can also do a database search of all women born after 29/03/1959 who are aged between 25 and 65 years – these women are in the eligible age range (remember to confirm eligibility through website, as they may have had screening done elsewhere).

Consultations related to screening may not arise in a woman’s routine interactions with their GP or GPN, but sampletakers need to have the conversation on both the benefits and limitations in this high-risk age group. Studies have identified that women who presented to the GP with gynaecological
conditions, such as menorrhagia or menopausal symptoms in the last five years were all up to date with screening. This indicates that consultations specific to gynaecological problems prompt both the clinician and the patient to consider cervical screening. However, screening is for people who are asymptomatic, and it is very important that it is not necessarily tied to conversations about genito-urinary symptoms, as this may lead women over 50 to believe that if all is well ‘down there’, that they do not need to attend for cervical screening.
Conversely, bringing up the topic of cervical screening may allow women to voice concerns about their sexual health that they may otherwise have kept to themselves. The genito-urinary symptoms of menopause (GSM), such as daily discomfort, itch, pain, and recurrent UTIs can cause significant physical and psychological distress, and yet women often feel uncomfortable about speaking to their doctor or nurse about them. Introducing the topic through discussion of cervical screening, and addressing concerns about fears of pain or discomfort in passing a speculum can provide the opportunity for offering appropriate and potentially life-changing management of these symptoms.
After menopause the vagina may be dry and atrophic, making introduction of the speculum more difficult. Choose an appropriate sized speculum and apply a water-soluble lubricant to the middle third of the shaft of the speculum (do not apply lubricant to the tip of the speculum as this can interfere with lab analysis). Remember one bad sampletaking experience can become a deterrent for a woman to return, so ensuring her comfort throughout the procedure is of paramount importance. If it is apparent from the initial consultation that she has symptoms related to vaginal atrophy,
then a course of vaginal oestrogen should be offered. The duration of the course is dependent on the severity of the symptoms, but a good rule of thumb would be to prescribe a pessary such as Vagifem or Vagirux twice weekly for six weeks, stopping five-to-seven days before the test is due in order to ensure that no trace of the pessary remains at the time of the test as it could interfere with the laboratory analysis. If the symptoms are very severe, it may be possible to continue with an oestrogen gel, such as Ovestin up to two days before the test is due.
Note: Previous breast cancer is not a contraindication to vaginal oestrogen in the vast majority of cases.
The cervical cell yield from the cervical screening test may be scanty. The absence of oestrogen causes the squamo-columnar junction (SCJ) to invert into the endocervical canal, making it more difficult to harvest cells from the columnar epithelium and transformation zone (TZ). If a cytology test is warranted, this leads to a higher probability of an unsatisfactory result. If a test needs to be repeated due to inadequacy, it is recommended to use local oestrogen PV as described above to encourage eversion of the SCJ, so that both the columnar epithelium and the entire transformation can be sampled.
Non-binary and trans people with a cervix have significantly lower screening rates than the general population. Sampletakers need to use inclusive language and indicate LGBT+ friendliness in the practice through the use of inclusive posters and behaviours. All practice staff should be encouraged to complete the HSELanD training modules and access the CervicalCheck quick reference guide for LGBT+ screening when available.
Waiting rooms are now open again so this is a good time to refresh practice posters and information. You can access
posters and other promotional materials at www.healthpromotion.ie for your waiting area.
HPV self-testing may become an alternative option for women who, for whatever reason, find it difficult to engage with a traditional clinic-based approach to cervical screening. The Netherlands is currently the only country in western Europe that offers self-sampling to all women who request it. Uptake of selfsampling there remained as low as 20 per cent throughout the pandemic, indicating that it has not been widely accepted by women despite its apparent convenience. Several countries, such as France and Denmark, offer self-sampling to certain under-screened populations. There are also ongoing pilots in the UK to assess this new method of screening. Further investigation within an Irish context is needed to assess if women would be willing to use this tool and to consider how it should be offered if implemented within our Irish cervical screening programme. There are many advantages to the woman of attending in person and having a holistic consultation around the benefits and limitations of screening with a well-trained clinician.
The forward-thinking implementation of the schools-based HPV vaccination programme along with the HPV primary screening programme puts Ireland ahead of many other countries and in a great position to aim for elimination of cervical cancer. We are fortunate to be in this position when we consider the global burden of this disease. However, we do know that older women are under-served and at increased risk and so we must increase our efforts to ensure that cervical screening is accessible, acceptable, and available for everyone who would benefit from it.
References on request
Isit with John and hold his hand through double gloves that slip from my sweat. He weeps as he tells me how lonely it is without Mary. She died alone in hospital. No visitors allowed.
“Do you think she was scared, nurse?” he agonises. My glasses steam silently with shared sadness.
The phone rings, interrupting the only face-to-face interaction John has had with another human in nearly a year. I ignore it. I try to connect with this 85-year-old widower through my mask, visor, and glasses. He cannot see the sadness I feel for him. The phone rings again. John holds my gloved hand tighter. It’s reception – “Your next two patients are getting agitated, they’re waiting for you nurse”. I ignore them. My door bangs. Let’s go, you have people waiting. I give John a gentle nod – go on, it’s ok to talk. My phone rings, it’s the trainee GP; “Nurse, can you come and look at this wound with me, I’m not sure what dressing to use.”
My breath draws short, my chest tight. Is this stress or could this finally be a visit from the virus? Maybe it’s this mask- it’s so tight. My face is cut. I wipe John’s tears and tell him to continue. He tells me how his wife of 70 years was zipped up and taken away to eternity. My hands are now working while my heart is listening. They draw vaccines into syringes, an action my hands do themselves by now. They buzz like bees beneath me. Working away. There are Covid-19 vaccines to give. I can tell John is comfortable with
me as he begins to weep harder. Someone walks into the room and interrupts again. “The other nurse is sick, she’s been sent home with Covid symptoms so you’ll have to double-up appointments”.
I take a breath and bring my gaze back to the crying man who sits before me. He apologises for keeping me. I can feel his grief magnify as he feels like a burden in my room. “No John, it’s fine. Tell me more”. I try to speak in soft tones, but the layers of protective wear drown out my condolences.
I hear the hungry cries of the newborn baby girl waiting outside my door. She waits for her first-ever vaccinations. She needs to be protected too. I take silent note of mum’s worried tone as she tries to sooth her. I need to make sure she is coping. There’s a lot of baby blues in this isolation. John starts to tell me about their first-born and how naturally his Mary took to motherhood. An earth mother he calls her. His sobs are halted by another phone call.
“Nurse, we have an elderly woman on the phone, she’s scalded herself with the

kettle. Her carer has Covid so she is home alone. Can you see her on your lunch break, the burns are awful.” No problem. I will make sure her wounds heal.

John squeezes my hand and tells me it’s nice to talk. It feels good. Well, better. I check his blood pressure and do some bloods, even though that was not the point of this visit today. I want to make sure his diabetes is under control. I don’t want him to end up in hospital. He might catch the virus there. There are no beds. Best to prevent rather than cure.
The door jolts open again. This time with force. It’s a patient. They are angry. They have been waiting for 20 minutes on their Covid-19 vaccine. There is shouting and abuse. “It’s not like you’re doing much anyways.” John quickly wipes away his grief. He sheepishly mutters “thank you nurse” as he shuffles his frail feet through the doorway. I blink away my tears. No time.
I bring mum in next. She is carrying a tiny bundle of pink hope. She goo’s at me, a new face is a rare sight for these children. Mum already has tears in her eyes. It is so hard. She hasn’t slept. I tell her she is strong. She is a woman. The phone rings. The newborn baby is startled and shrieks
ensue. The world has stopped for a short time, but I think about the future. The phone rings again.
My name is Clare. I’m a general practice nurse (GPN). Like all nurses, I am well used to the oppressive gaslighting of our profession. Unequal pay and unsafe staffing is the baseline for nurses in Ireland. But we answered ‘Ireland’s call’ when the time came.
There are many misconceptions about general practice nursing. We are the chief vaccinators in the country and the backbone of health screening and health promotion in Ireland. We spend our days doing immunisations, cervical screening, chronic disease management, asthma, COPD, diabetes and cardiovascular disease, nurse prescribing, medication administration, phlebotomy, weight management, smoking cessation services, women’s health, men’s health, dermatology, wound management, travel vaccinations, cryotherapy, aural care and ear irrigation, triage, health promotion, counselling, as well as follow-up, referrals, and liaising with other healthcare professionals, conducting clinical audits, developing practice protocols, coding of health conditions, maintenance of emergency equipment and are involved in practice staff education.
When Covid-19 hit, GPs switched to mostly phone consultations, but we practice nurses never culled our clinics. We continued to see all our patients, run GP clinics, and put ourselves at risk. Our workload increased and we stood with our other nursing colleagues on the frontline just as much as anyone else. Although we did not zip up body bags on the wards, we did make sure that we kept the rest of the country well in an effort to avoid this fate, whilst also trying to treat sick patients to keep them away from the doors of acute hospitals.
Then the primary Covid-19 vaccination programme was rolled out and I can assure you each and every

single GPN was at the forefront of this nationwide. The first day those patients walked through our doors, aged 85 and up, we soothed their fears and reassured them that everything was going to be okay. We spoke softly. We were gentle and tactile through suffocating layers of PPE. We wiped the tears of our elderly patients as they told us just how lonely it had been in their ‘cocoons’. And then we carried on and vaccinated half of the population. We stayed into the night at the end of each clinic when we had extra vaccines to be used up, we called every patient we knew and we walked the streets to find arms to vaccinate when everybody else was done. We answered 'Ireland's call' and gave up our holidays and festive celebrations and came to work to give the population hope of new beginnings.
I am aware the GPs (doctors) were paid for each vaccine given in their clinics, but we weren't. GPNs were not paid with the money that GPs received for their nurses' work. For us, this is not about the money. GPNs nationwide are shocked and perplexed as to how they've been excluded in this 'recognition' when they have been integral in leading this country through this pandemic. Babies were still vaccinated, new mums were soothed, the elderly were cared for, the dying comforted, wounds were healed, and the country was given protection against Covid-19. But because we are 'privately employed', we were not frontline workers? Did we not put ourselves at enough risk? Did we not work hard enough? Did we not do a good enough job? How is it that we are now excluded, but just weeks ago we were told we were "healthcare heroes" when we were yet again asked to disrupt our annual leave to come in and vaccinate you and your colleagues and their families and the rest of the country? Why is it that Minister Pascal Donoghue tells Ireland that we are not frontline workers?
AUTHOR: Priscilla LynchGENERAL PRACTICE NURSES HAVE REACTED WITH ANGER AND DISGUST AT BEING OMITTED FROM THE GOVERNMENT’S PANDEMIC BONUS PAYMENT OF €1,000, AND LABELLED AS NONFRONTLINE HEALTHCARE WORKERS
General practice nurses (GPNs) around the country have condemned the Government’s decision that GPNs are not to be included in the special once-off Covid-19 frontline healthcare worker ‘recognition payment’ of €1,000.
The tax-free payment is being given to public service health and ambulance workers, those seconded or assigned to the HSE (for example: Defence Forces staff seconded/assigned to HSE testing centres), supernumerary students who were required to perform training in clinical sites, and staff in private sector nursing homes and hospices affected by Covid-19, but not to ‘private’ healthcare staff, such as GPs, GPNs, and pharmacists.
The Irish General Practice Nurses Educational Association (IGPNEA) heavily criticised Minister for Finance Paschal Donohue TD, who said on RTE 1’s Prime Time current affairs and news programme (Thursday, 20 January) that GPNs were not frontline healthcare workers.
Mary Jordan, IGPNEA Chairperson,said that the IGPNEA membership was furious with the Minister’s remarks, which she said completely misrepresented the vital role that GPNs have played, and continue to play, in battling the Covid-19 pandemic.
“I would call on the Minister to withdraw his remarks, on national tv, which show a complete lack of respect, and a total lack of understanding, of the work that GPNs do on the frontline of the health service during this most challenging of times,” she said.
Ms Jordan went on to highlight the critical element which GPNs delivered in terms of the country’s vaccination roll-out. “The Minister is obviously completely unaware that 100 per cent of Covid-19 vaccines given to the most vulnerable cohort of patients, those aged 80 years and over, were delivered in general practice; that 50 per cent of the vaccines delivered across the country to all age groups were delivered by general practice nurses,” adding that the IGPNEA membership had let their feelings be known to her in relation to the “ill-informed views that the Minister expressed”.
“GPNs are proud to say that we continued to care for our patients throughout this pandemic. When patients presented with injuries that required immediate attention we did not stop to ascertain their Covid vaccine status prior to treatment. When patients attended with exacerbations of lifelimiting conditions too fearful to attend a hospital
We worked tirelessly to keep ourselves and our patients and colleagues safe in order to keep our practices open. General practice nurses are also to the fore of many other elements of healthcare delivery across the country, including delivering community-based healthcare across multiple settings, and supporting GPs across the country.”
Carlow GPN and lecturer Theresa Lowy-Lehnen said it was clear from Minister Donohue’s comments that
the role of the GPN is misunderstood and undervalued. “GPNs worked throughout the pandemic, providing face to face and direct contact care for patients. They were lead practitioners in the roll-out, organisation and delivery of the Covid-19 vaccination programme in primary care and played a key role in shielding secondary care services throughout the crisis. Within Irish general practice 90 per cent of an estimated 20 million episodes of patient care are completed and managed annually without requiring
onward referral. GPNs carry out much of this work.” She maintained that “the role of GPNs as frontline healthcare practitioners throughout the pandemic should be recognised and valued by Government and t hey should be acknowledged and included in the frontline healthcare workers bonus payment”.
Many GPNs took to twitter to make their views known. South Dublin GPN Karen Canning voiced her disgust and anger and pointed out that 99 per cent of a GPN’s work is on behalf of the HSE, as did Mayo GPN Orla Loftus Moran.

Many GPs also supported calls for the pandemic bonus to be extended to GPNs. Dublin GP Dr Conor McGrane made a plea to Government TDs to extend the €1,000 to GP receptionists and nurses. "They were right at the front with ill people breathing/ coughing feet away. Not highly paid and deserve this so much.”
Cork city GP Dr Sarah Sheehan, said: “How could you say a group of workers who gave 50 per cent of all Covid vaccines (particularly the rush for boosters pre Christmas) are not really frontline workers?”

THE ROLE OF GPN s AS FRONTLINE HEALTHCARE PRACTITIONERS THROUGHOUT THE PANDEMIC SHOULD BE RECOGNISED AND VALUED BY GOVERNMENTTheresa Lowy-Lehnen Orla Loftus Moran AUTHOR: Priscilla Lynch
GENERAL PRACTICE NURSES PLAY A KEY ROLE IN IDENTIFYING RISK FACTORS FOR OSTEOPOROSIS, AND IN THE DIAGNOSTIC, TREATMENT, AND SUPPORT PATHWAY FOR PATIENTS

At present it is estimated that 300,000 people in Ireland have osteoporosis. One-infour men and one-in-two women aged over 50 years will develop a fracture due to osteoporosis in their lifetime and the so-called ‘silent’ disease can also affect children.
The impact of osteoporosis on qualityof-life can be profound as a result of loss of independence, decreased self-esteem, distorted body image and depression. Vertebral fractures also significantly impact on activities of daily living, such as washing, dressing, and walking.
However, fractures and osteoporosis are preventable in most people and treatable in the majority, so general practice nurses (GPNs) need to be alert to the risk factors in their patients, to ensure that those at risk of developing osteoporosis are assessed for the disease.
Key risk factors include advanced age, low body weight, prior fracture, having a condition or medication that causes bone loss, eating disorders, family history, alcohol use and smoking. Women are more at risk, and women lose up to 30 per cent of their overall bone mass whilst going through the menopause.
Unfortunately in many cases osteoporosis diagnosis is only made after a person has suffered a low impact ‘fragility’ fracture.
Over the last number of years, wider availability of DEXA scans has increased the likelihood that people at risk of osteoporosis may be diagnosed before they
develop fractures so those in this category should be encouraged to obtain a DEXA scan, which remains the gold standard screening modality for the diagnosis of osteoporosis. GPs now have direct access to DEXA scan referral through the HSE.
As well as looking out for risk factors, GPNs can support patients through diagnosis and treatment, while general lifestyle advice is also important.
The primary goal of osteoporosis therapy is to reduce the risk of fracture. A comprehensive osteoporosis treatment programme should include a focus on proper nutrition, exercise, and safety issues
to prevent falls that may result in fractures. In addition, medication to slow or stop bone loss, increase bone mineral density (BMD), and reduce fracture risk may be prescribed. The main medications and procedures used to treat osteoporosis include:
Bisphosphonates;

Hormone replacement therapy (HRT) or contraceptive pill;
Selective oestrogen receptor modulators (SERMs);
Monoclonal antibodies;
Parathyroid hormone (PTH);
Testosterone;
Vertebroplasty (a non-surgical treatment involving a needle with ‘bone cement’ inserted into the fractured body of the
vertebrae under imaging guidance); Kyphoplasty (a surgical treatment involving a balloon being placed into the fractured vertebrae, followed by ‘bone cement’ being injected into the balloon).
Checking up on osteoporosis patients to determine their tolerance of and compliance with their medications and to monitor for any potential side-effects is important. As previously reported in NiGP, drug holidays during the Covid-19 pandemic led to reduced BMD and a rise in fractures, and consequently pain and disability, in some osteoporosis patients. Research has shown that follow-on denosumab administered after nine-to-12 months versus the advised six months results in a 50 per cent decrease in BMD gains, with rapid BMD loss even after one month, and early risk of vertebral fracture and, later, other fractures.
Aside from referral for diagnosis and medical treatment, there are a number of other supports that can be provided in general practice for those at risk of/ diagnosed with osteoporosis.
GPNs should assess the patient's knowledge of osteoporosis and provide education regarding dietary intake (such as increasing calcium and vitamin D intake, recognising foods high in calcium, and limiting carbonated sweetened drinks, which are usually high in phosphorus) and exercise.
The Irish Osteoporosis Society (IOS) website contains a range of education and support material for healthcare providers on osteoporosis.
Eating foods rich in calcium and vitamin D can make a difference, not only for bone health but overall health.
Foods that have significant amounts of calcium in them include all dairy products – milk, cheese, and yoghurt. Vegans are at higher risk of bone loss as are those in the 5 per cent of people in Ireland who are lactose intolerant, but green vegetables, especially kale, Collards, and okra are excellent sources of calcium. Fish, such as tinned salmon and sardines, are also excellent choices, as well as fortified breakfast cereals.
Sunlight is an excellent source of vitamin D, but sun safety awareness and wearing appropriate levels of sunscreen is key. Good sources of vitamin D are fortified milks, fatty fishes – salmon, tuna, and mackerel, plus egg yolks. Calcium and vitamin D supplementation may also be necessary.
There are plenty of types of exercise, particularly weight-bearing exercise, that are beneficial for those with osteoporosis, but improving strength, bone density, and balance should be part of any exercise programme, notes the IOS. Pilates incorporates all of these, so is an excellent option for osteoporosis, it says.
to be modified as they can put a strain on the bones of the spine.
Strengthening exercises using bands, free weights or bodyweight can help increase bone density and these exercises would be progressed slowly. Pilates can also help strengthen the muscle groups needed to help improve posture. Strengthening of the thigh muscles, the muscles around the hip, and tummy muscles is important to improve bone density and to help prevent falls.
People with osteoporosis are advised to avoid strong and sudden twisting and bending exercises, particularly when using weights so these exercises may need to be altered, whereas exercises that involve arching or extending the spine can be helpful. Pilates also incorporates balance and coordination exercises that can help prevent falls, it can help prevent fractures in people with osteoporosis. Pilates instructors should be able to tell patients which exercises to avoid and modify other exercises.
Pilates classes are now found in a variety of settings. It is worth considering there to be two types of Pilates –recreational (as in a gym setting) and clinical (as in a physiotherapy clinic or other health setting).
Recreational Pilates may not be suitable for those with osteoporosis due to class sizes and quick progression of exercises and is often more suitable for younger people. Clinical Pilates is sometimes called rehabilitative Pilates and the instructor would usually be a health professional, such as a chartered physiotherapist who would be qualified to treat those with osteoporosis. Although Pilates exercise done under the correct supervision can be helpful for those with osteoporosis, there are some exercises that should be avoided and others that need
If someone has osteoporosis and wants to attend Pilates, they should find a class with a small number of attendees (preferably fewer than 10 in a class) to make sure they get good supervision during the class. It is usually a good idea to have a oneto-one session with the instructor prior to the class so that they can do an assessment with regards to ability and discuss any scan results, any medical conditions, and any medications the person is taking.
There are several things you can advise osteoporosis patients to do to reduce the risks in their home.
Install handrails on stairs and grab bars in bathrooms.
Get rid of throw rugs and electrical cords lying across floors, which can be easily tripped over.
Make sure halls, stairways, walkways, and porches are well lit.
Wear comfortable shoes with flat heels and non-slip soles.
Have non-slip mats in front of sinks. See www.irishosteoporosis.ie for more information and support materials.
GPN s SHOULD ASSESS THE PATIENT'S KNOWLEDGE OF OSTEOPOROSIS AND PROVIDE EDUCATION REGARDING DIETARY INTAKE ... AND EXERCISE
• Available in 800 IU tablets and 4000 IU tablets
• Daily flexible dosing of 800 IU - 4000 IU Vitamin D3
ABBREVIATED PRESCRIBING INFORMATION:
Desunin (colecalciferol), 800 IU & 4000 IU Tablets.

Please refer to Summary of Product Characteristics (SmPC) before prescribing.
Indications, Dosage and Administration: Desunin 800 IU: Desunin 800 IU is indicated for the prevention and treatment of vitamin D deficiency in adults and adolescents.
In addition to specific osteoporosis treatment of patients who are at risk of vitamin D deficiency, preferably in combination with calcium
Desunin 4000 IU: Desunin 4000 IU is indicated for the treatment of vitamin D deficiency in adults and adolescents.
Vitamin D deficiency is defined as serum levels of 25-hydroxycolecalciferol (25(OH)D) < 25 nmol/l.
Recommended dose: One tablet per day.
The dose should be adjusted dependent upon desirable serum levels of 25-hydroxycolecalciferol (25(OH)D), the severity of the disease and the patient´s response to treatment. The daily dose should not exceed 4000 IU.
Pediatric population
The safety and efficacy of Desunin in children under 12 years have not been established.
Dosage in hepatic impairment
No dose adjustment is required.
Dosage in renal impairment
Desunin should not be used in patients with severe renal impairment (see section 4.3 of the SmPC).
Administration: The tablets can be swallowed whole or crushed. The tablets can be taken with food.
Presentation: Tablets
Contraindications:
• Diseases and/or conditions resulting in hypercalcaemia or hypercalciuria.
• Nephrolithiasis
• Nephrocalcinosis
• Hypervitaminosis D
• Hypersensitivity to the active substance or to any of the excipients listed in section 6.1 of the SmPC
Warnings and precautions:
Desunin should be prescribed with caution to patients suffering from sarcoidosis due to risk of increased metabolism of vitamin D into its active form. These patients should be monitored with regard to the calcium content in serum and urine. During long-term treatment, serum calcium levels should be followed, and renal function should be monitored through measurements of serum creatinine. Monitoring is especially important in elderly patients on concomitant treatment with cardiac glycosides or diuretics (see section 4.5 of the SmPC) and in patients with a high tendency to calculus formation. In case of hypercalciuria (exceeding 300 mg (7.5 mmol)/24 hours) or signs of impaired renal function the dose should be reduced, or the treatment discontinued.
Desunin should be used with caution in patients with impairment of renal function and the effect on calcium and phosphate levels should be monitored. The risk of soft tissue calcification should be taken into account. In patients with severe renal insufficiency, vitamin D in the form of colecalciferol is not metabolised normally and other forms of vitamin D should be used.
The content of vitamin D (800 IU or 4000IU) in Desunin should be considered when prescribing other medicinal products containing vitamin D. Additional doses of vitamin D should be taken under close medical supervision. In such cases it is necessary to monitor serum calcium levels and urinary calcium excretion frequently. Excipients: Desunin contain sucrose, isomalt and sodium. Patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine.
This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodium-free’.
Interactions with other medicinal products and other forms of interactions:
Thiazide diuretics reduce the urinary excretion of calcium. Due to the increased risk of hypercalcaemia, serum calcium should be regularly monitored during concomitant use of thiazide diuretics.
Concomitant use of phenytoin or barbiturates may reduce the effect of vitamin D since the metabolism increases.
Excessive dosing of vitamin D can induce hypercalcaemia, which may increase the risk of digitalis toxicity and serious arrhythmias due to the additive inotropic effects. The electrocardiogram (ECG) and serum calcium levels of patients should be closely monitored.
Glucocorticoid steroids may increase vitamin D metabolism and elimination. During concomitant use, it may be necessary to increase the dose of Desunin tablets.
Simultaneous treatment with ion exchange resins such as cholestyramine or laxatives such as paraffin oil may reduce the gastrointestinal absorption of vitamin D.
Fertility, pregnancy and lactation:
Fertility - There are no data on the effect of Desunin on fertility. However, normal endogenous levels of vitamin D are not expected to have any adverse effects on fertility.
Pregnancy - Desunin should be used during pregnancy, only in the case of a vitamin D deficiency. Desunin is not recommended during pregnancy in patients without a vitamin D deficiency as the daily intake should not exceed 600 IU vitamin D.
Studies in animals have shown reproductive toxicity of high doses of vitamin D (see section 5.3 of the SmPC).
There are no indications that vitamin D at therapeutic doses is teratogenic in humans.


Breast-feeding - Vitamin-D can be used during breast-feeding. Vitamin D3 passes into breast milk. This should be considered when giving additional vitamin D to the child.
Undesirable effects:
Very common (≥1/10): None
Common (>1/100, <1/10): None
For details of uncommon, rare and very rarely reported adverse events and those of unknown frequency, see SmPC.
Reporting of adverse reactions:
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via HPRA Pharmacovigilance, Earlsfort Terrace, IRL – Dublin 2; Tel: +353 1 6764971; Fax: + 353 1 6762517. Website: www.hpra.ie. E-mail: medsafety@hpra.ie.
Adverse reactions/events should also be reported to the marketing authorisation holder at the email address: pv.ireland@viatris.com or phone 0044(0)8001218267. Legal
THIS NEW EXPERT TEXTBOOK ON DERMATOLOGY IN PRIMARY CARE WAS FORMALLY LAUNCHED AT THE RECENT PRIMARY CARE DERMATOLOGY SOCIETY OF IRELAND (PCDSI) 2022 ANNUAL MEETING
BOOK TITLE:
Textbook of Primary Care Dermatology

AUTHOR: Dr David Buckley and Dr Paola Pasquali
PUBLISHER: Springer
REVIEWER: Dr Karen Enright
As a GP with more than a little interest in dermatology, this book by the guru of primary care dermatology Dr David Buckley, and Dr Paolo Pasquali, was my favourite Christmas present.
Dr Buckley is a leader in Irish community dermatology with the Kerry Skin Clinic, which treats all manner of medical, surgical, and allergic skin disease and is an outstanding example of what can be achieved in primary care with training, expertise and passion.
I cannot recommend this textbook enough. All GPs, general practice nurses and other healthcare professionals with (or without) an interest in dermatology would benefit from having a copy of this book on their shelf.
It is written from the perspective of a GP, focusing on the practical management of common, and some uncommon, skin conditions, what we can safely manage ourselves, and how and when to phone a friend.
Skin complaints represent at least 15
per cent of GP consultations, and often times they are an ‘add on’ at the end of the consultation – “oh, while I am here doc, can you check this mole/rash/lump for me”.
As Dr Buckley points out, skin disease should be considered as relevant and prioritised the same way as any other medical complaint and we need to remind ourselves and patients of this, because a life-threatening skin cancer could be missed at a treatable stage.
Dr Buckley makes a great point in the chapter on ageing skin; the burden of skin disease is much higher in the elderly and with life expectancy increasing year on year – based on trends predicted by the Central Statistics Office (CSO) in Irelandthe number of people aged over 65 years is likely to double or even triple over the
next 35 years. Therefore, there will be an ever-increasing demand for skin care in the elderly in the community going forward.
Dermatology tends to be a marmite subject among GPs; you either love it or hate it. Undergraduate training is significantly lacking in dermatology and so unless they are lucky enough to get a postgraduate dermatology post, skin disease can be much of a mystery to many GPs.
Dr Buckley makes the reassuring statement that when it comes to undiagnosed skin eruptions, it is much more likely to be an unusual presentation of a common problem than a rarity in the subtext of a dermatology textbook. So a broad knowledge of the basics of medical dermatological presentations with a fundamental plan for each is likely to get the majority of presentations managed.
When it comes to surgical dermatological presentations of pigmented and nonpigmented skin lesions in Dr Buckley’s words: “There is only one rule when assessing suspicious pigmented (or nonpigmented) lesions – if in doubt cut it out or refer to a colleague with more experience in skin recognition.”
The chapter on lesion recognition is a great resource with a flowchart from the Primary Care Surgical Association (PCSA) describing management of new or changing lesions.
Dr Buckley’s four-point warning signs for skin cancer ‘new cancers do show’ is a very useful and memorable acronym to alert doctors and patient to lesions that should
Skilfully combining 50 years of scientific knowledge & expertise.
Oilatum, a proven treatment for eczema and related dry skin conditions.


Medically Proven
Comprehensive range for adults and children
Trusted for generations

Oilatum Emollient* contains light liquid paraffin. Used to treat itchy, irritating dry skin conditions including eczema and dermatitis, particularly when they affect large areas of your body. Oilatum Junior Flare-up* contains light liquid paraffin, benzalkonium chloride and triclosan. Relieves itching, reduces redness associated with eczema flare-ups in children and helps protect against further drying. Avoid contact of the undiluted product with the eyes and the skin. If your condition does not improve, or if you experience any unwanted effects, stop using the product, consult your pharmacist or doctor. FOR EXTERNAL USE ONLY. *Fire Hazard: product burns more easily. Do not smoke or go near naked flames; clothing and bedding with this product dried on them can catch fire easily. Washing clothing and bedding may reduce product build-up but not totally remove it. A copy of the summary of product characteristics is available on request. PA 126/322/001 (Oilatum Emollient 63.4% Bath Additive) PA 126/323/001 (Oilatum Junior Flare Up bath Additive). Medicinal products not subject to medical prescription. PA Holder: Clonmel Healthcare Ltd., Waterford Road, Clonmel, Co. Tipperary. Also available, Oilatum Soap Bar, an emollient cleanser suitable for everyday cleansing for dry and sensitive skin. Always read the label. Date prepared: October 2021. 2021/ADV/OIL/103H

be viewed with suspicion: New – a new growth sore, freckle or mole that has appeared in the past six-to-12 weeks.
Changing – a growth, sore, freckle or mole that is changing in size, shape or colour.
Different – a growth, sore, freckle or mole that looks different from any other ‘ugly duckling’ sign.
Sore – a growth, sore, freckle or mole that is sore, tender, bleeding or itchy.
Acne is one of the most common dermatological presentations in general practice, with 90 per cent of teenagers developing it at some stage and around half of these continuing to suffer as an adult. Dr Buckley describes a stepwise approach to management with flow charts, rationale behind each treatment, and what to do if not responding.
Included is a prescribing guide, courtesy of Dr Deirdre Lundy; one of Ireland’s leading experts in women’s health, describing acne as generally mediated through progesterone, which can be a likely side-effect of secondgeneration oral contraceptive pills (OCP). Therefore, it is recommended to switch to a fourth-generation OCP initially and if not improving increase to a higher oestrogen dose OCP. The examples of each of these with trade names are listed, making this a most useful and practical reference flowchart.
Dr Buckley also describes how to safely treat acne in pregnancy, which can be challenging.
Included in the chapter on eczema is something I have never read before; a table listing over-the-counter (OTC) emollients from most oily to least. This is incredibly helpful when suggesting the most appropriate emollient or soap substitute for a patient, when invariably they have already tried a few, and this gives the expertise to explain why their eczema/ dermatosis/xerosis has not responded and what might be a better choice.
Included in the allergic skin diseases chapter is a table describing how to distinguish various forms of dermatitis; atopic, irritant contact dermatitis; and allergic contact dermatitis from clinical features. Then most helpfully when and what allergy test is required to confirm the diagnosis; from IgE blood tests, skin patch or skin prick testing – which speaking for myself has always been a subject of confusion. Following is a table of the common allergens tested on a patch test (type 4 allergy, eg, allergic contact dermatitis) and aeroallergens and ingested allergens on skin prick testing (type 1 hypersensitivity, eg, urticaria). Although any type of drug can cause any type of dermatological eruption, a list of the most common suspects is provided to give some clarity when trying to eliminate iatrogenic aetiology in those difficult to treat chronic urticaria presentations.
Warts are a very common and often frustrating presentation in primary care for the doctor and the patient. Although they are harmless (aside from anogenital warts, which are associated with increased risk of cancer) and will inevitably resolve within two years, they can cause distress and embarrassment especially in children and young adults when on the face or hands. A list of treatment options when the first-line OTC topical ointments have not been successful is provided. This includes the obvious cryosurgery, but also the less obvious 5 per cent imiquimod, topical podophyllotoxin, topical glutaraldehyde, and a very effective treatment used in
Canada, cantharidin, which may become available in Ireland in the future. Equally practical information is a list of the salicylic acid-based topical treatments with the percentage of salicylic acid present in the preparation from ‘Vericaps plasters’ at 12 per cent to ‘Verrugon ointment’ at 50 per cent, meaning if patients want to stick with topical therapy, an evidence-based suggestion can be given with stepwise increase in concentration of salicylic acid. About 75 per cent of warts will resolve with topical salicylic acid when used properly.
Now for a subject close to my heart, skin surgery. A strap line for all primary care surgical-trained GPs is, “If in doubt, cut it out.” As Dr Buckley describes, training in dermoscopy can often help with diagnosis of pigmented and non-pigmented skin lesions, but if an accurate diagnosis cannot be made, the safest option is to gain histology with an incisional or excisional skin biopsy. In Dr Buckley’s words, “any changing or new mole over the age of 40 should be viewed with suspicion and referred to a colleague with more experience in skin lesion recognition.” Equally, although most melanomas are pigmented, amelanotic melanomas can present as a non-pigmented macule or nodule and “any new or changing lesion, regardless of colour, should be viewed with suspicion and biopsied unless a confident, clinical, named diagnosis can be made based on history, examination, and dermoscopy”.
Dr Buckley outlines best practice for simple skin surgery with pathways for biopsy and safeguarding tips including: “most skin surgery errors are made with the pen not the knife”. Other tips include stretching the skin perpendicular to Langer lines when doing a punch biopsy to enable easy closure, wound healing, and reduced scar formation.
Something very useful as a quick reference for any GP performing skin surgery is the outline of the PCSA guidelines for patients taking anticoagulants and skin surgery, for patients taking antiplatelets, DOACs or warfarin.
A STRAP LINE FOR ALL PRIMARY CARE SURGICAL TRAINED GPs IS, 'IF IN DOUBT, CUT IT OUT'
There is also a great tip on local anaesthetic and adrenaline use when performing skin surgery.
The chapter on photoageing was most interesting. Dr Buckley makes an interesting point that most ageing of the face and hands is likely to be due to accumulation of photodamage from UV exposure. Actinic keratosis, solar lentigos, elastosis, skin thinning, wrinkling, telangiectasia, purpura, and of course NMSA all increase with age, but if you compare the skin on the face to that of the buttocks – it is evident there is a vast influence from UVR.
There are various treatments including topical tretinoin, hydroquinone, vitamin C and E, chemical peels, and aesthetic injectables, such as botulinum toxin and intradermal fillers, which can address some of the ageing effects of the skin. However, the most basic and effective is prevention rather than cure by the application daily of SPF factor 30 or greater all year round.
Dr Buckley debunks some of the myths surrounding SPFs. Anything over SPF 50 does not confer any additional benefit and adds an additional chemical load as the higher the SPF in chemical sunscreens, the higher the concentration of sun-filtering chemicals. For this reason physical sunscreens may be more suitable for people with sensitive or allergy prone skin. Chemical sunscreens may be poorly tolerated by patients with rosacea, lupus or photodermatosis. Of course, here in not-sosunny Ireland the majority of us are vitamin D deficient in the winter months. The use of high-factor SPF may interfere with the skin’s ability to metabolise vitamin D in the summer, therefore Dr Buckley suggests considering a vitamin D supplement, especially in those aged over 50 years.
The chapter on leg ulcers gives a really straightforward approach when addressing a leg ulcer. Dr Buckley recommends that basic advice to the patient should not be underestimated, which includes encouraging walking and avoiding
standing, elevating the feet and ankles for two hours in the morning and evening, and maintaining a healthy weight, diet, and level of hydration.
In clinic the next practical step is to perform a pedal pulse check and ankle brachial pressure index (ABPI) if these are weak, impalpable or difficult to assess. Based on the ABPI index, the recommendation of grades of compression or referral to a vascular surgeon is described.
He then gives a visual step-by-step demonstration of how to apply compression bandages. And beyond that a description of what type of dressing is suitable for each type of ulcer whether it be infected, complicated/resistant, non-infected exudative or simply weeping eczema. I will admit the world of dressings has always been a mystery to me, leaving that rather sheepishly in the hands of my esteemed nursing colleagues!
Dr Buckley outlines timeframes where ulcers less than 1cm should heal over six-to-12 weeks with compression bandages, with advice on when to change the dressings.
A tip I will most definitely use to aid diagnosis of pityriasis versicolour is to place sellotape over a small plaque. This common patchy scaly hyper or hypopigmented eruption is caused by a proliferation of a normal skin commensal Malassezia. Using the sellotape will reveal an area of scales in the exact shape as the skin lesion. Once treated with oral or topical anti fungals the infection is no longer present, but the pigmentary changes can persist for six-to-12 weeks.

The chapter on vascular tumours and melanocytic naevi in children is very useful. Dr Buckley describes the different vascular tumours: Capillary haemangioma (strawberry naevus), capillary malformations (port wine stain), and nevus flammeus (stork mark and angel kisses). He describes the clinical features, the natural history and when to
refer to dermatology and why. Of interest the advice is to refer infants with over five capillary haemangiomas for a liver ultrasound, because of increased risk of liver haemangiomas. Also, presence of capillary haemangiomas in the midline increases risk of airway haemangiomas.
Melanocytic naevus acquired before the age of two are deemed congenital and over the age of two, acquired. He describes the appearance and histological features of the different types of melanocytic naevus; junctional, compound, and intradermal.
There is also a chapter on Covid-19 skin disease and the merits of telemedicine in dermatology, which is very topical.
A special mention also needs to be given to the patient information leaflets. These are so practical, useful, and time-saving for GPs to have to hand. There is everything from consent forms for minor surgery, hand-care tips for dermatitis, how to safely use topical steroids with fingertip units, to managing scabies and head lice. With Dr Buckley’s permission I will have a copy of all these sitting to hand in my clinic!
I have read my fair share of dermatology textbooks and this is the best; most comprehensive, practical and GP-focused guide I have come across. Thank you Dr Buckley and Dr Pasquali for sharing your wealth of experience and information. The GPs and GPNs who read it, and their dermatology patients, will be all the better for it.

To order a copy of this book go to: https://link.springer.com/ book/10.1007/978-3-030-29101-3.
The PCDSI 2022 Annual Meeting took place virtually on 4-5 March. There will be coverage of the meeting in the next edition of NiGP. Please see www.pcdsi.com for more information.

Consilient Health Ireland are delighted to announce the relaunch of their new website www. consilienthealth.ie.
The aim of the redesign was to help healthcare professionals and patients find the information and resources they require to facilitate best standards in healthcare.
Resources to support bone health include the Eat Well for Bone Health booklet by Paula Mee, recipes high in calcium and vitamin D, and general hints and tips on bone health. Information on women’s health
topics include the contraceptive missed pill guide, advice on starting the pill, and general guidance on other contraceptive-related topics. There is also a section on managing your menopause.
For healthcare professionals, resources include the patient management guide on contraceptive pills as well as the 'meetings and webinars' page where healthcare professionals can register for all of the future CH webinars and access previous webinars in the areas of women’s
Windzor Pharma are delighted to announce the launch of GlucoRX Aidex to the Irish Market. GlucoRx Aidex is a continuous glucose monitor available for all patient types.
The sensors are small and secure and can be used on the arm or the abdomen. Each transmitter has a lifespan of three years and each sensor lasts up to 14 days. All data is submitted from the sensor to the GlucoRx Aidex app making it easy to track glucose levels during the day.


For more information, training or to order please contact: orders@windzorpharma.com.
Transmitters and sensors are available through UDW and Uniphar and PCO. Sensor GMS code 85241.
health and bone health.
“Covid-19 has transformed how we communicate. Consilient Health remain committed to providing information to healthcare professionals and patients that is medically accurate and relevant and is now more accessible through www.consilienthealth. ie,” said Deirdre Kelly, Consilient Health Ireland Country Manager. Resources are downloadable, but hard copies may also be requested via our office team at irishoffice@ consilienthealth.com.
2 - Mediocre (7)
3 - Resolution (8)
4
5 - Worried and nervous (7)
6 - Become tense (7)
7 - Conditions (5)
11 - Not absolute (8)
12 - Liked by many people (7)
13 - Reply (7)
15



