Major Depressive Disorder (MDD) can turn people into shadows of their former selves

References:
1. Al-Harbi K et al. Patient Prefer Adherence 2012; 6: 369-388.
2. Keller MB. J Clin Psychiatry 2005; 66(Suppl 8): 5-12.
3. Rush AJ et al. Am J Psychiatry 2006; 163(11): 1905-1917.
Date of preparation: September 2021
Item code: CP-246536
Up to 30% of patients with MDD fail to respond to their first antidepressant therapy.1,2
More than 2 in 3 responders fail to reach remission – with remission rates declining with each treatment step:3
• 31% achieve remission with a second treatment
• 13% achieve remission with a fourth
It’s time to step out of the shadow of MDD.
Janssen Sciences Ireland,
Ringaskiddy, IRL - Co. Cork P43 FA46
Barnahely,
Hoping for better mental health and neurology care this year
A message from Priscilla Lynch, Editor
Welcome to the latest edition of Update Psychiatry and Neurology.
As we begin this new year, the Covid-19 pandemic is continuing to have a substantial impact on our lives.
While there is hope on the near horizon given the emergence of an apparently less virulent variant (omicron), coupled with the success of vaccination and ongoing development of new treatments, the impact on the nation’s mental health and healthcare service provision will be felt for quite some time to come.
As Prof Brendan Kelly outlines in this issue, evidence to date indicates that the combined effects of the pandemic itself and the public health restrictions it necessitates have resulted in approximately one person in every five in the general population experiencing significantly increased psychological distress.
Furthermore, while there continue to be encouraging developments in neurology and psychiatry knowledge, both at home and abroad, basic service provision during the pandemic remains one of the biggest challenges facing those working in the field.
Mental health and neurology professionals in already long under-resourced and understaffed structures in Ireland are doing their best to provide ongoing services to patients. Waiting lists for community-based psychology services and CAMHS and neurological rehabilitation services remain appalling, with the impact of the medical recruitment and retention crisis very apparent.

But, as ever, the need for learning and sharing of information continues.
This issue features a wide range of clinical and research update articles to help increase your knowledge base of brain disorders.
On the medical conference front, there is exclusive coverage from the College of Psychiatrists of Ireland’s latest Winter Meeting.
Focusing on Irish research, there is an article on the latest successes of FutureNeuro, the SFI Research Centre dedicated to developing new technologies and solutions for the treatment, diagnosis, and monitoring of neurological diseases, which highlights the Centre’s important ongoing work.
And, in a very welcome development, this issue features an article explaining how, from this month, the neurology service at Tallaght University Hospital will become an expert centre for both atypical Parkinsonism and cerebellar ataxias and hereditary spastic paraplegias within the European Reference Network for Rare Neurological Diseases (ERN-RND).
This issue also contains a number of expert management articles on bipolar disorder, anxiety, schizophrenia, medication overuse in migraine, and progressive supranuclear palsy, which outline the most effective treatment approaches, as well as overview articles on motor neurone disease, narcissistic personality disorder, and the evidence to date on the benefits of mindfulness.
There are also timely pieces on the mental health impact of post-Covid-19 syndrome, and tackling neurophobia in Ireland, particularly in general practice.
The College of Psychiatrists of Ireland has just launched a position paper on the development of services for personality
disorders, the details of which are outlined in this issue. It is estimated that a diagnosis of borderline personality disorder features in up to 20 per cent of clinical presentations to mental health outpatient clinics in Ireland, and the lack of dedicated services for these patients is leaving them without access to treatments that would greatly support their quality-of-life, and pushing them further to the margins of our health service and society as a whole, the College said.
The College has also just published a position paper on assisted dying, an issue which will shortly be the focus of a Special Oireachtas Committee set up to examine the Dying with Dignity Bill (2020). A naturally controversial topic, opinions are mixed among the general public and medical profession about the best approaches in this area. The College has warned that allowing doctors to assist in the suicide of their patients represents a fundamental and irreversible shift in medicine’s philosophy and practice, and that it is not compatible with good medical care. The College further warns that its introduction in Ireland could place vulnerable patients at risk: “Euthanasia creates the risk that many people will die from treatable psychological distress and mental illness.” See page 3 for more details.
All-in-all, this is a packed edition of Update that should hopefully prove interesting and useful to all our readers.
Thank you to all our expert contributors for taking the time to share their knowledge and advice for the betterment of patient care.
We always welcome new contributors and ideas and suggestions for future content, as well as any feedback on our content to date. Please contact me at priscilla@mindo.ie if you wish to comment or contribute an article. ■
1 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
Editor Priscilla Lynch priscilla@mindo.ie
Sub-editor Emer Keogh emer@greenx.ie
Creative Director Laura Kenny laura@greenx.ie
Advertisements Graham Cooke graham@greenx.ie
Administration Daiva Maciunaite daiva@greenx.ie
Update is published by GreenCross Publishing Ltd, Top Floor, 111 Rathmines Road Lower, Dublin 6 Tel +353 (0)1 441 0024 greencrosspublishing.ie
© Copyright GreenCross Publishing Ltd 2022
The contents of Update are protected by copyright. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means – electronic, mechanical or photocopy recording or otherwise – whole or in part, in any form whatsoever for advertising or promotional purposes without the prior written permission of the editor or publisher.
Disclaimer
The views expressed in Update are not necessarily those of the publishers, editor or editorial advisory board. While the publishers, editor and editorial advisory board have taken every care with regard to accuracy of editorial and advertisement contributions, they cannot be held responsible for any errors or omissions contained.
GreenCross Publishing is owned by Graham Cooke graham@greenx.ie
2
Contents 03 College of Psychiatrists of Ireland position paper on assisted dying 04 College of Psychiatrists of Ireland position paper on services for personality disorders 05 Narcissistic personality disorder (NPD): An overview 08 College of Psychiatrists Winter Meeting coverage 11 A recap on schizophrenia 13 Progressive supranuclear palsy: An update 15 The common manifestations of anxiety disorders 17 Irish hospitals join European network of expert centres for rare neurological diseases
Diagnosis and treatment of bipolar affective disorder 20 Migraine: Medicationoveruse and medicationoveruse headache 24 An update on mindfulness: What is the evidence? 27 An overview of motor neurone disease 30 Combating neurophobia in Irish healthcare 34 The psychiatric impact of post-Covid-19 syndrome 36 An update from FutureNeuro SFI Research Centre 38 Expert exercise prescriptions for Parkinson’s disease
18
College of Psychiatrists of Ireland warns against introduction of assisted dying legislation in Ireland
Euthanasia is illegal in Ireland and the Irish Medical Council forbids participation in the deliberate killing of a patient. Other jurisdictions have moved to permit euthanasia in one form or other, with some more restricted and others very broad.
In Ireland, as in many other countries, the question is increasingly arising as to whether doctors may become involved in ending patients’ lives, either directly (euthanasia) or indirectly (physician-assisted suicide), together known as PAS-E. A related question is whether the law should ever compel them to do so.
Not surprisingly, this is a controversial topic and opinions are mixed among the general public and the medical profession about the best approaches in this area.
The issue will shortly be the focus of a Special Oireachtas Committee set up to examine the Dying with Dignity Bill (2020).
There are medical, psychological, and social implications to the direct and indirect ending of the lives of seriously ill and vulnerable people. Allowing doctors to assist in the suicide of their patients represents a fundamental and irreversible shift in medicine’s philosophy and practice according to the College of Psychiatrists of Ireland.
The College has warned that PAS-E is not compatible with good medical care and that its introduction in Ireland could place vulnerable patients at risk. “Euthanasia creates the risk that many people will die from treatable psychological distress and mental illness.”
Acknowledging the psychological distress often associated with the end of life, and because of the unintended consequences of permitting euthanasia and assisted suicide,
the College recently (20 December 2021) published a position paper on this area which sets out what it sees as some key issues regarding the introduction of assisted dying in Ireland. This document was prepared by the Human Rights and Ethics Committee of the College and approved by the College Council in September 2021.
“In keeping with national and international experts in palliative care we believe that euthanasia is not necessary for a dignified death and on the contrary may diminish personal dignity.”
Key issues outlined by the College in its paper include that:
Assisted dying is contrary to the efforts of psychiatrists, other mental health staff, and the public to prevent deaths by suicide.
It is likely to place vulnerable people at risk – many requests for assisted dying stem from issues such as fear of being a burden or fear of death rather than from intractable pain. Improvements in existing services should be deployed to manage these issues.
While often introduced for patients with terminal illness, once introduced assisted dying is likely to be applied more broadly to other groups, such that the numbers undertaking the procedure grow considerably above expectations;
The introduction of assisted dying represents a radical change in Irish law and a long-standing tradition of medical practice, as exemplified in the prohibition of deliberate killing in the Irish Medical Council ethics guidelines.
Commenting, Consultant Liaison Psychiatrist Dr Eric Kelleher, a member of the College and contributing author to the position paper on assisted dying, said: “We are acutely aware of the sensitivity of
this subject, and understand and support the fact that dying with dignity is the goal of all end of life care. Strengthening our palliative care and social support networks makes this possible. Not only is assisted dying or euthanasia not necessary for a dignified death, but techniques used to bring about death can themselves result in considerable and protracted suffering.
“Where assisted dying is available, many requests stem, not from intractable pain, but from such causes as fear, depression, loneliness, and the wish not to burden carers. With adequate resources, including psychiatric care, psychological care, palliative medicine, pain services, and social supports, good end of life care is possible,” he said.
Dr Siobhan MacHale, Consultant Liaison Psychiatrist, a member of the College and contributing author to the position paper on assisted dying, added: “Once permitted in a jurisdiction, experience has shown that more and more people die from assisted dying. This is usually the result of progressively broadening criteria through legal challenges because, if a right to assisted dying is conceded, there is no logical reason to restrict this to those with a terminal illness.”
She continued: “Both sides of this debate support the goal of dying with dignity, but neither the proposed legislation nor the status quo (as evidenced by both clinical experience and the power of this debate) is sufficient. It is imperative for the Irish people to continue to demonstrate leadership as a liberal and compassionate society in working together to achieve this.”
The full position paper is available at www.irishpsychiatry.ie.
3 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
New CPI position paper on personality disorder services
The College of Psychiatrists (CPI) recently published a new position paper titled Develop–ment of Services for Treatment of Personality Disorder in Adult Mental Health Services
It is estimated that a diagnosis of borderline personality disorder features in up to 20 per cent of clinical presentations to mental health outpatient clinics in Ireland.
A lack of dedicated services for people with personality disorders is leaving individuals diagnosed without access to treatments that would greatly support their qualityof-life, and pushing them further to the margins of our health service and society as a whole, the College said.
To begin a conversation toward establishing a more robust system of care for those affected by these disorders, a dedicated special interest group within the CPI put together this position paper, which identifies the level of unmet need in Ireland and makes recommendations for the future development and improvement of services.
Often further co-occurring mental health needs present, such as addiction, depression or anxiety, with those with personality disorder having a higher likelihood of emergency presentations and suicidality. The wider effects on people’s lives and on society as a whole can be also seen: Higher health service utilisation, poorer physical health outcomes, interactions with the criminal justice system, and greater economic toll. Delivering evidence-based treatments as a first-line for people with personality disorders would help to alleviate significant harm for both the individual and costs for health services, the paper says.
The position paper looks to begin with the following four key actions:
1. Identify the prevalence and level of unmet need of personality disorders in Ireland, with a focus on adult mental health services.
2. Review the scientific evidence on treatments for personality disorders and international treatment guidelines.
3. Establish the current level of service provision for personality disorder in Ireland.
4. Make recommendations to the HSE and CPI for the further development of personality disorder treatment in Ireland.
Existing services
In support of their aim of improving service provision, the Personality Disorder Special Interest Group has previously conducted a survey of College members, which sought to identify existing service offerings in adult mental health services for the treatment of personality disorders. Only 57 per cent of respondents stated that they had an evidencebased treatment in their service while a worrying 9 per cent of respondents were unaware of any specific interventions offered. Nearly half of respondents identified a lack of resources as the main obstacle to delivering an appropriate service for people with personality disorder.
The group also hopes for greater collaboration with service users in the design and delivery of services that support patient autonomy and choice, hope, and trusting therapeutic relationships between patient and clinician.
Despite the existence of several wellevidenced and cost-effective treatments for personality disorders, the newest mental health policy for Ireland, ‘Sharing the Vision: A Mental Health Policy for Everyone’, which was launched in 2020, does not specifically refer to pathways or services for those with personality disorders at all.
To address the concerning lack of treatments for personality disorders on offer in Irish mental health services, the paper makes the following recommendations:
Implementation of the recommendation of ‘A Vision for Change’ to provide both localised
and specialist services including evidencebased treatments of people with personality disorders and to further commission a National Clinical Programme for personality disorders to further develop the provision of services within Ireland.
The establishment and funding of specialist consultant medical psychotherapist posts that will in turn provide the expertise and leadership necessary to manage specialist personality disorder services.
To ensure the expectation that services for people with personality disorders will be offered throughout the country and not just in a few locations or pilot sites.
To develop a wider educational programme about personality disorders, broadening knowledge and awareness of personality disorder within the health service more broadly and also associated agencies such as social care and the criminal justice system.
The establishment of a mechanism that would include the patient voice in the development of training and services.The full paper can be accessed at www.irishpsychiatry.ie
Background
The Personality Disorders Special Interest Group was established by the College for members interested in the aetiology, treatment and management of personality disorders in adults and emergent personality disorders in adolescents. It aims to promote learning and information sharing on the management of personality disorders, to help support educational and training initiatives for clinicians working with personality disorders, and to advocate for better service provision for adults with a personality disorder or emergent personality disorders amongst adolescents. Its Chair is Dr Paul Matthews.
For more information about the Personality Disorders Special Interest Group, please email hmurray@irishpsychiatry.ie.
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 4
Narcissistic personality disorder (NPD): An overview
AUTHOR: Theresa Lowry-Lehnen, RGN, GPN, RNP, PhD, Clinical Nurse Specialist and Associate Lecturer Institute of Technology Carlow
Narcissistic personality disorder (NPD) is a complex personality disorder often detected with other affective and personality disorders.1 Affected people have unstable and intense emotions and a distorted image of ‘self’. NPD is a disorder in which the individual is overly preoccupied with vanity, prestige, power, and personal adequacy, lacks empathy, and has an exaggerated sense of superiority. This excessive sense of importance and superiority, combined with a preoccupation with success and power do not reflect real self-confidence. The individual often has a deep sense of insecurity and fragile self-esteem. 3
The legend of Narcissus, a character in Greek mythology from which the term narcissism derives (Narcissus fell in love with his own reflection in a pool of water), has become one of the most prototypical myths of modern times. However, narcissism has become a defining feature of the modern era and interest in the concept has captured the imagination of the public, media and literature. This has been paralleled by a growing body of academic interest and empirical research, particularly in the fields of psychology, social science and cultural studies. Within psychiatry, the concept of narcissism has evolved from early psychoanalytic theorising to its official inclusion as a personality disorder in psychiatric nomenclature.6
Extensive literature regarding aetiological theories of narcissism exists, predominantly from psychoanalytic and psychodynamic perspectives, but more recently from social learning theory and attachment research.6 The widespread use of the concept of pathological narcissism
as a distinct personality type by clinicians influenced by psychoanalysts such as Kernberg and Kohut, and psychologists such as Millon, led to the introduction of NPD into the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM)-III in 1980. The NPD construct was further refined and modified as it evolved through DSM-III-R (1987) and DSM-IV (1994) on the basis of the empirical findings of an increasing number of psychological studies identifying narcissism as a personality trait. These shifts in the diagnostic criteria for the disorder however were criticised for losing some of the more dynamic variables present in its phenomenological manifestations. The diagnostic criteria for NPD in DSM-5 are focused on characteristics of grandiosity and entitlement rather than more vulnerable manifestations of the disorder. However, it is generally accepted that at least two subtypes or phenotypic presentations of pathological narcissism can be differentiated: Grandiose or overt and vulnerable or covert narcissism.6
Presentation of NPD
DSM-5 describes NPD as a pervasive pattern of grandiosity, fantasy or behaviour, need for admiration and lack of empathy, beginning by early adulthood and indicated by at least five of the following. The individual: 2
Has a grandiose sense of self-importance, eg, exaggerates achievements, expects to be recognised as superior without actually completing the achievements;
Is preoccupied with fantasies of success, power, brilliance, beauty, or perfect love;
Believes that they are ‘special’ and can only be understood by or should only associate with other special people or institutions;
Requires excessive admiration;
Has a sense of entitlement, such as an unreasonable expectation of favourable treatment or compliance with his or her expectations;
Is exploitative and takes advantage of others to achieve their own ends
Lacks empathy and is unwilling to identify with the needs of others;
Is often envious of others or believes that others are envious of them;
Shows arrogant, haughty behaviours and attitudes.
Narcissism is a trait, but can also be a part of a larger personality disorder. Not every narcissist has NPD, because narcissism is a spectrum. People who are at the highest end of the spectrum are those
5 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
NPD is a disorder in which the individual is overly preoccupied with vanity, prestige, power and personal adequacy, lacks empathy, and has an exaggerated sense of superiority
that are classified as NPD, but others with narcissistic traits may fall on the lower end of the narcissistic spectrum. While everyone may show occasional narcissistic behaviour, true narcissists frequently disregard other people or their feelings and also do not understand the effect that their behaviour has on other people. 5
Narcissists can initially be very charming and charismatic and don’t always show negative behaviour straight away. Narcissists like to surround themselves with people who feed into their ego and build relationships to reinforce their ideas about themselves, even if these relationships are superficial. 5
People with NPD have difficulty handling perceived criticism and can:
Become impatient or angry when they don’t receive special treatment;
Have significant interpersonal problems and easily feel slighted;
React with rage or contempt and belittle others to make themselves appear superior;
Have difficulty regulating emotions and behaviour;
Experience major problems dealing with stress and adapting to change;
Feel depressed and moody because they fall short of perfection;
Have secret feelings of insecurity, shame, vulnerability and humiliation.
Risk factors
The aetiology of NPD is not fully understood. However, as with personality development and other mental health disorders, the causes of NPD are likely complex and multifaceted and NPD may be linked to environment, genetics and neurobiology.7 Traits such as aggression, reduced tolerance to distress, and dysfunctional affect regulation are prominent in people with NPD.
Developmental experiences, negative in nature, being rejected as a child, and a fragile ego during early childhood may contribute to the occurrence of NPD in adulthood. In contrast, excessive praise, including the belief that a child may have extraordinary abilities, may also lead to NPD.1 ‘Grandiose’ and ‘vulnerable’ narcissism are two different types of narcissism that have common traits, but which can arise from different childhood experiences. People with grandiose narcissism were most likely treated as if they were superior or better than others during childhood and these expectations can follow them into adulthood. Those with grandiose narcissism are aggressive, dominant, and exaggerate their importance. They are very self-confident, lack sensitivity and tend to be elitist. 5 Vulnerable narcissism is usually the result of childhood neglect or abuse. People with this behaviour are more sensitive and narcissistic behaviour helps to protect them against feelings of inadequacy. Even though they go between feeling inferior and superior to others, they feel offended or anxious when other people do not treat them as if they are special. 5
Pathological narcissism
The more encompassing term ‘pathological narcissism’ has been used to better reflect personality dysfunction that is fundamentally narcissistic, but allows for both grandiose and vulnerable aspects in its presentation.4 Individuals with pathological narcissism express many difficulties of identity and emotion regulation within the context of significant interpersonal relationships. While previous research has established some of the interpersonal impact on those in a close relationship with someone exhibiting traits of pathological narcissism, no qualitative studies existed until recently. In 2020, a significant qualitative study on living with pathological narcissism took place, and involved 2,219 relatives of people reportedly high in narcissistic traits. 3 Participants in this
study described ‘grandiosity’ in their relative as the need for admiration, displaying arrogance, entitlement, envy, exploitativeness, grandiose fantasy, selfimportance, interpersonal charm, and a lack of empathy. They also described ‘vulnerability’ of their relative as contingent self-esteem, hypersensitivity and insecurity, affective instability, emptiness, rage, devaluation, hiding the self, and having a victim mentality. Grandiose and vulnerable characteristics were commonly reported together by 69 per cent of respondents in this study. Participants also described perfectionistic, vengeful, antisocial, suspicious, and paranoid features in the individual. Living with a person with pathological narcissism can be marked by experiencing a person who shows large fluctuations in affect, oscillating attitudes, and contradictory needs, and these findings have implications for diagnosis and treatment in that the initial spectrum of complaints may be misdiagnosed unless the complete picture is understood. 3
Diagnosis
A sense of entitlement is common in people with narcissism. They often believe that they are superior to others, deserve special treatment, people should be obedient to their wishes, and they may become rude or abusive when they do not receive the treatment they feel they deserve. Manipulative or controlling behaviour is another common trait. A narcissist will at first try to please and impress, but eventually, their own needs will always come first. When relating to other people, narcissists will try to keep people at a certain distance in order to maintain control and exploit others to benefit themselves. One of the most common signs of a narcissist is a need to boost their ego, to feel appreciated and receive validation from others. The narcissist is unwilling or unable to empathise with the needs, wants, or feelings of other people. 5 They commonly have an expectation that others will automatically go along with what he or she wants and have an inability to
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 6
recognise or identify with the feelings, needs, and viewpoints of others. Envy of others or a belief that others are envious of them and hypersensitivity to insults whether real or imagined, criticism, or defeat, possibly reacting with rage, shame, and humiliation is common. 5
Generally, narcissists do not recognise their disorder or seek help as it does not fit the self-image they have of themselves, and they may need the encouragement of others to seek professional help. Diagnosis of NPD typically is based on signs and symptoms, a physical exam, a thorough psychological evaluation that may include filling out questionnaires, and the NPD criteria as listed in DSM-5 8
Obtaining an accurate history can be somewhat challenging with NPD, given the variability of the presentation. Individuals can be well related and high functioning, but they can also be aggressive and challenging patients.1 The diagnosis of NPD like other personality disorders requires evaluation of long-term patterns of functioning. A careful evaluation of the different aspects of a person’s life and an understanding of the person’s childhood development can assist in the evaluation and diagnosis of NPD.1
A standard psychiatric interview is often used to make a diagnosis of personality disorders. Other instruments may measure the severity of NPD, such as the five-factor narcissism inventory that looks at the five aspects of general personality. There are approximately 148 questions on the fivefactor inventory. Another measure that may be useful is the Narcissistic Personality Inventory. NPD is usually present with other mood disorders. Once a diagnosis is established, it is important to discuss the diagnosis because of several challenges that will be present. It is equally important to treat ongoing symptoms of co-occurring affective disorders.1
Treatment options
No standardised pharmacological or psychological treatment has been
established for people with NPD and there is no effective, known cure.1 Psychotherapy is often recommended, which helps the patient better understand their problems. This may bring about a change in their attitudes, resulting in better behaviour. Psychotherapy may involve cognitive behavioural therapy (CBT), family therapy or group therapy. CBT helps the patient
including selective serotonin reuptake inhibitor (SSRIs) and serotoninnorepinephrine reuptake inhibitors (SNRIs), have been used. Risperidone, an antipsychotic, has shown benefit in some patients and mood stabilisers such as lamotrigine. The prognosis depends on the severity of the disorder and the degree to which people who seek treatment recognise the problems within themselves, and aim to change the maladaptive aspects of their personality.
identify negative beliefs and behaviours, and replace them with healthy and positive ones. Psychotherapy aims to help patients build their self-esteem and acquire realistic expectations of themselves and other people. For some of the more distressing aspects associated with NPD, medication may be required. Antidepressants,
References
1. Mitra P, Fluyau, D. (2021). Narcissistic personality disorder. Available at: www. ncbi.nlm.nih.gov/books/NBK556001/
2. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders 5th ed (DSM-5). Arlington
3. Day N, Townsend M, Grenyer B. (2020). Living with pathological narcissism: a qualitative study. Bord Personal Disord Emot Dysregul 7, 19. https://doi.org/10.1186/ s40479-020-00132-8
4. Russ E, Shedler J. (2013). Defining narcissistic subtypes. In: Ogrodniczuk JS, editor. Understanding and treating pathological narcissism: American Psychological Association; 2013. p. 29-43
5. Brennan D. (2020). Narcissism:
Living with somebody who has NPD Family members and close contacts of people with NPD often describe them as controlling, egotistical, and dissatisfied with what anybody around them does. No matter what happens, the narcissist will blame others and make them feel guilty for their problems. They are described as having short fuses, losing their temper at the slightest provocation, or turning their backs and giving people the ‘silent treatment’. Some can be physically and sexually abusive. The emotional and physical damage caused by somebody with NPD can be severe and learning to become more confident and assertive can help protect those living with a person with NPD from long-term harm. 3
Symptoms and signs. In WebMD. Available at: www.webmd.com/mentalhealth/narcissism-symptoms-signs
6. Yakeley J. (2018). Current understanding of narcissism and narcissistic personality disorder. B J Psych Advances, 24 (5), 305-315. doi: 10.1192/bja.2018.20
7. Mayo Clinic. (2021). Narcissistic personality disorder. Symptoms and causes. Available at: www.mayoclinic.org/ diseases-conditions/narcissistic-personalitydisorder/symptoms-causes/syc-20366662
8. Mayo Clinic. (2021). Narcissistic personality disorder. Diagnosis and treatment. Available at: www.mayoclinic. org/diseases-conditions/narcissisticpersonality-disorder/diagnosis-treatment/ drc-2036669 0
7 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
No standardised pharmacological or psychological treatment has been established for people with NPD and there is no effective, known cure
College of Psychiatrists of Ireland, Winter Conference, virtual, 4-5 November 2021
 ALL REPORTS BY VALERIE RYAN
ALL REPORTS BY VALERIE RYAN
Service
capacity for managing eating disorders to be ‘exceeded’ for some time to come
The disproportionate impact of the Covid-19 pandemic on people at risk of eating disorders and the pressures of a spike in referrals and the volume of people seeking care in outpatient and acute inpatient settings, were underlined by leading consultant psychiatrists in the field at the latest Winter Conference of the College of Psychiatrists of Ireland (CPI).
The Irish experience of clinicians reporting high volumes in outpatient clinics during the pandemic has been in line with international health services.
“But even with adaptations, service capacity for assessment and treatment is going to be exceeded for some time,” Consultant Child and Adolescent Psychiatrist and Clinical Lead of the HSE Child and Adolescent Regional Eating Disorder Service (CAREDS) for Cork and Kerry, Dr Sara McDevitt, told conference attendees.
“Telehealth has been suitable for some aspects of care but certainly not all. Active waiting is now an essential part of what we do. And this has had a huge strain on doctor-patient relationships,” she said during the session on ‘Eating disorder care in a changed landscape – what have we learned toguide our next steps?’
Prior to the pandemic, services were confident they could manage referral, assessment, and treatment in a timely manner.
However, timelines have worsened over the past six months. Services did not have the capacity to take on the large volumes of people immediately, she said.
Dr McDevitt’s comments on the impact of Covid-19 and a large increase in the number of presentations were echoed by Consultant Liaison Psychiatrist, Dr Siobhan MacHale, Associate Clinical Professor, RCSI, who outlined the impact of the pandemic on the inpatient setting of an acute hospital – Beaumont Hospital in Dublin. Dr MacHale, presenting on eating disorder management in the general hospital, referred to a large increase in eating disorder admissions noted during 2021.
The acute hospital services were not just for patients presenting with eating disorders, such as anorexia nervosa, avoidantrestrictive food intake disorder (ARFID), bulimia nervosa, binge eating disorder, but also the impact of, for example, obesity in terms of patients’ presentations and the impact of their overall health journey. Non-specified eating disorders were also seen by the service.
Each of these required a slightly different approach. But the component that brought them into an inpatient setting was where the medical consequences of their eating disorder resulted in significant malnutrition and/or metabolic disturbances.
About two-thirds of patients would have significant cardiac complications at the time of presentation to the hospital.
She recommended the need to follow the MARSIPAN (Management of Really Sick Patients with Anorexia Nervosa) guidelines, which were about to be updated, originally developed by a multi-professional group working in the field due to the number of patients with anorexia nervosa who had been presenting in hospitals and dying within a number of days.
Up to 2017, she told College members, the service was seeing nine to 12 cases of anorexia nervosa per year, until 2020 when there was a significant drop to six admissions. However, 2021 had triggered a rapid escalation reaching 21 admissions in the first 10 months, on extrapolated data, with 24 expected during the year.
She stressed the challenges for the services in the face of increased presentations
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 8
including resource difficulties and the impact of Covid-19, which had reduced staff availability.
Also during the Winter Conference, results from a study by Dr Jahan Khan and
colleagues at St Patrick’s Mental Health services in Dublin, “clearly indicate that the majority of patients attending the eating disorder service were negatively impacted by the pandemic,” with many reporting worsening eating disorder symptoms.
Their study, presented as part of the NCHD poster section, included all adult patients attending the eating disorder service during the year before the Covid-19 pandemic. They believed a follow-up study would be helpful to establish long-term impact.
Recruitment and retention plan crucial for expansion of specialty of psychiatry
President of the CPI, Dr William Flannery, re-iterated a call for over 800 consultant psychiatrists to be appointed in psychiatry by 2030, and urged publication of a crucial draft HSE/National Doctors Training and Planning (NDTP) unit plan for recruitment retention, in his opening remarks to the College’s Winter Conference 2021.
Speaking at the meeting, which took place on 4-5 November on a virtual basis, Dr Flannery referred to the recommendations for additional consultants, outlined in the NDTP unit medical workforce planning report on the specialty of psychiatry, and pointed out that progress has been slow.
He added that the document in train on recruitment and retention would be crucial to “the challenges we all face in the workplace”.
Training is the core of the College’s remit and although costing an estimated €1.9 million a year to fund adequately, he advised members that the College was due to receive €1.3 million for training which had represented an increase on previous funding.
On the Mental Health Act, Dr Flannery said it had to be amended and was currently with the Attorney General’s office. The Law Committee of the College was due to meet
to identify four or five key areas from the College’s perspective.
He complimented the Faculty of Medical Psychotherapy for its position paper, endorsed by the College. “That position paper is the development of services for treatment of personality disorder in adult mental health services. So now we have a position paper, the College can use this to get the direction we want,” said Dr Flannery.
Dr Flannery also paid tribute to the work of colleagues, who had various roles in policies and operations, for their hard work and for working with him.
Preventive measures urged to safeguard staff and patients in psychiatric settings
A need for preventive measures and improved reporting to safeguard staff and patients from violent incidents in psychiatric workplace settings has been highlighted in separate NCHD studies, presented at the latest Winter Conference of the CPI.
‘Zero violence or zero seclusion. Which is more acceptable in our hospitals?’, aimed to determine the number, nature, and characteristics of violent incidents and other incidents in a secure forensic hospital in Ireland.
Conducted at the Central Mental Hospital (CMH), Dublin, by Dr Kezanne Tong and colleagues, a total of 320 incidents were recorded between March 2019 and August 2021.
Since March 2020, the researchers observed an upward trend in the number of physical violence incidents perpetrated by patients. The number of incidents of actual physical assault had also increased during the study period.
They noted that the current lack of
admission beds in psychiatric services in Ireland, together with the very limited numbers of psychiatric ICU beds, “likely means that patients may be more unwell by the time they are admitted.”

In turn, this could have an effect on, firstly, the proportion of admissions that were involuntary, and, secondly, on the rates of seclusion and restrictive practice, as patients were more unwell on admission.
Restrictive practices must be used in accordance with the law, but were necessary
9 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
at times to prevent serious harm to patients and staff in psychiatric hospitals, according to the research. Any review of mental health legislation or the code of practice in relation to restrictive practice “must reflect on the
Westmeath Mental Health Services, and Dr Elaine Walsh, Mayo Mental Health Services, ‘Experiences of, and attitudes to, the reporting of violence in the workplace by mental health care staff’, recommended
sense of futility amongst staff; more than half feeling that violent incidents are preventable in the first instance and 70 per cent feeling that reported incidents are not properly investigated.”
The study found that 91 per cent of 67 respondents to the survey reported verbal abuse; 31.3 per cent recorded physical assault; 14.9 per cent had suffered sexual violence; and a further 13.4 per cent experienced racial harassment in a 24-month period. “A staggering 4.5 per cent of these reported that violence occurred daily.”
primary need for the safety of staff and patients in psychiatric hospital settings”.
A separate study considered the issue of reporting levels of violent incidents in psychiatric settings.
Presented by Dr Joanne Fegan, Longford/
further work was needed in the prevention of workplace violence as well as improvements in reporting and investigating of incidents when they did occur.
It was clear from the response to an online survey that: “There is a high degree of non-reporting of violence with an apparent
It was not unreasonable to speculate that the recorded figure of 6,690 violence incidents in 2018 and 2019, from the State Claims Agency, fell short of the reality as this figure represented the collation of the official National Incident Management System forms that were filled in by staff regarding violent incidents, added the study.
Large scale trials considering therapeutic use of low-dose psychedelics in depression
Latest trials and research into therapeutic use of controlled low-dose psychedelics, such as psilocybin, ketamine, and substituted amphetamines in mainstream psychiatry, was outlined at the CPI Winter Conference.
A session on ‘Ketamine and psychedelics in psychiatry: Pipers at the gates of dawn?’ highlighted new research into the psychopharmacology and possible therapeutic potential of psychedelics for treatment of resistant psychiatric conditions.
College members heard of preclinical studies that were elucidating neurobiological mechanisms, which may underlie their antidepressant effects.
Prof Andrew Harkin, Associate Professor of Pharmacology, School of Pharmacy and Pharmaceutical Sciences, Trinity College Dublin (TCD), detailed their
psychopharmacology, brain connectivity, and “new research in neuroscience that is prompting a resurgence in the potential of these drugs for the clinic”.
On the pharmacology of ketamine, he said that at some anaesthetic doses, the antidepressant actions of the drug was noted.
A series of trials where these observations had been reported included published results of a trial of 18 patients, with treatmentresistant major depressive disorder, who showed robust and rapid response to intravenous ketamine for up to a week following infusion of a sub-anaesthetic dose.
These studies had prompted a lot of drug discovery and development effort. This had culminated in the US FDA approval, in March 2019, of the intra-nasal delivery of esketamine for treatment-resistant depression.
Prof Veronica O’Keane, TCD and Tallaght Psychiatry Services, discussed tryptamines in her talk on ‘Psilocybin as a treatment for depression and as a way to look through the windows of consciousness to the connected brain’.
She said studies focusing on psilocybin had exceeded those of other psychedelics. Most studies worldwide were looking at psilocybin as a treatment for depression.
Details of the first randomised double-blind, placebo-controlled trial of psilocybin for the treatment of resistant depression by the Tallaght Psychiatry Service were presented.
Prof Declan McLoughlin, TCD and St Patrick’s University Hospital, Dublin, followed up with a discussion on: ‘Is there a role for ketamine in routine clinical practice?’

Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 10
In turn, this could have an effect on, firstly, the proportion of admissions that were involuntary, and, secondly, on the rates of seclusion and restrictive practice, as patients were more unwell on admission
A recap on schizophrenia
AUTHORS: Dr Niall Duffy, Registrar in Psychiatry, Saint John of God Hospital, Stillorgan, Co Dublin; and Dr Stephen McWilliams, Associate Clinical Professor, School of Medicine and Medical Sciences, University College Dublin, and Consultant Psychiatrist, Saint John of God Hospital
(two or more voices discussing the individual among themselves);
CASE REPORT
Johnny is a 28-year-old man referred by his GP to a psychiatric crisis assessment team. It seems his family are concerned about some of his beliefs and recent behaviours. He has been working from home since the Covid-19 pandemic restrictions began in early 2020. A few months ago, Johnny started to hear voices of his colleagues telling him they believe his university qualifications to be fake and that he will never amount to anything in life. Lately they have accused him of fraud and have threatened to inform the guards. These voices are clearly heard out loud and have become relentless; he is understandably frightened by them.
Schizophrenia is characterised by a fundamental distortion in several mental modalities including perception, thought, belief, self-experience, cognition, affect and volition. It carries a lifetime risk of around 1 per cent and presents most commonly in late adolescence to early adulthood. The incidence in males and females tends to be equal, but onset tends to be earlier in males. For a diagnosis of schizophrenia to be made, the psychosis cannot be attributable to mania or depression, an organic brain disease, or intoxication with or withdrawal from substances.
The causes of schizophrenia have been studied for many decades and appear to encompass several different risk factors including genetics, developmental issues and environmental influences (such as cannabis and other illicit substances). Combinations of genes seem to make individuals more susceptible to developing schizophrenia, with family and twin studies highlighting an increased risk where a first-degree relative has been diagnosed. But not everyone with
He starts to worry that his colleagues are monitoring his movements via computer surveillance and he fears for his safety. He covers his webcam with tape and keeps his phone switched off, making it difficult for his employers to contact him. He stops attending occasional face-to-face meetings in case his colleagues use this as an opportunity to plant a bug on him. Soon he stops leaving the house completely. His parents finally persuade him to attend the crisis team and the psychiatrist forms the view that he is experiencing a first episode of psychosis suggestive of emerging schizophrenia. Johnny agrees to be admitted to a local psychiatric hospital for assessment and treatment.
(d) Persistent delusions of other kinds, (delusions being fixed, false beliefs that cannot be explained by religious or cultural contexts);
(e) Persistent hallucinations in other modalities;
(f) Thought disorder (where the link between one thought and the next is disrupted);
(g) Catatonic behaviour, such as mutism or posturing;
(h) Negative symptoms, with a change in the quality of an individual’s personal behaviour, which can be remembered as the ‘5As’:
Affective flattening (poor eye contact, reduced facial expression);
Alogia (poverty of speech, latency or delay in the response to questions);
Avolition (lack of drive with evidence of emotional withdrawal);
these risk factors will develop schizophrenia. Indeed, the ‘stress-vulnerability’ model dictates that increased levels of pressure in everyday life, combined with risk factors, may increase the likelihood of an emerging psychotic episode.
Diagnosis
The diagnosis of schizophrenia, using criteria outlined in the World Health Organisation’s (WHO’s) International Classification of Diseases (ICD-10), is based on clinical judgement in the context of a clear understanding of the symptoms comprising specific criteria. Specifically, at least one of (a), (b), (c) or (d) below – or two of (e), (f), (g) or (h) below – must be evident for the diagnostic criteria to be met:
(a) Thought echo, insertion, withdrawal or broadcast;
(b) Delusions of control, impulse or passivity (ie, of being under the control of external forces);
(c) Auditory hallucinations, which are usually running commentary (describing the individual’s behaviour) or third-person
Anhedonia/asociality (reduced interests or activities, and impaired relationships with family members or friends);
Attention deficits (social inattentiveness).
In the ICD-10, the psychotic symptoms must be present most of the time for a period of at least one month. If the symptom criteria are met, but last for less than a month, then schizophrenia should not be diagnosed initially. The ICD-10 categorises schizophrenia into nine different subtypes – paranoid, hebephrenic, catatonic, undifferentiated, post-schizophrenic depression, residual, simple, other and unspecified – however, these categories will soon be obsolete as we herald the ICD-11, which is due to be adopted into practice from January 2022. Here, the subtypes of schizophrenia are to be removed and replaced by groups of dimensional and longitudinal descriptors which allow a more individualised description of the presentation of the illness and its course over a period of time.
The symptoms of schizophrenia have generally remained unchanged in the ICD-11, with core symptoms involving persistent hallucinations,
11 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
persistent delusions, thought disorder and experiences of influence, passivity or control. A formal diagnosis will require at least two out of a total seven symptoms (one of which must be a core symptom) present for at least one month.
The diagnosis of schizophrenia using the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5) differs somewhat, with an individual needing to meet a defined set of criteria in order to receive a diagnosis.
Treatment
The treatment of schizophrenia, like all other psychiatric disorders, follows a biopsychosocial approach. Treatment in an inpatient setting may be required with the first presentation of a psychotic illness and in more severe presentations, allowing access to robust multidisciplinary assessment and a calm environment with limited stimulus. The UK National Institute for Health and Care Excellence (NICE) guidelines are one among several trusted sets of clinical practice guidelines (CPGs) for the treatment of schizophrenia. NICE recommends offering an oral antipsychotic in the first instance, with patient involvement as much as possible to provide information on efficacy and the potential sideeffect profile (noting that this may not always be possible where the presentation is severe).
Antipsychotic medications are divided into first-generation (FGA) and second-generation (SGA) varieties. Many FGAs have been available since the early 1950s and include haloperidol, zuclopenthixol, chlorpromazine and sulpiride. Common side-effects include sedation, weight gain, prolonged QTc, hyperprolactinaemia, and extrapyramidal signs (acute dystonia, akathisia, Parkinsonism, and tardive dyskinesia).
SGAs have mostly been used since the early 1990s and include olanzapine, risperidone, paliperidone, quetiapine, amisulpride and aripiprazole. Some SGAs have a greater metabolic side-effect burden (exceptions being amisulpride and aripiprazole) leading to an increased risk of metabolic syndrome. Clozapine first became available in the 1970s and remains the most efficacious SGA. It is reserved for cases of treatment-resistant
schizophrenia due to the potentially fatal side-effect of agranulocytosis, which ultimately quelled its widespread use until a Clozapine Patient Monitoring Service (CPMS) was established in the 1990s. The CPMS regularly monitors the white cell count of every clozapine patient and ensures that it is safe to use. Other potential side-effects include sedation, weight gain, constipation, hypersalivation, cardiomyopathy, and seizures.
Both FGAs and SGAs are effective in the treatment of positive symptoms (experiences that are present when they should not be) such as delusions, hallucinations and thought disorder. According to the Maudsley Prescribing Guidelines, there is little evidence favouring either antipsychotic group in the treatment of negative symptoms (experiences that are not there when they should be), such as the 5As. Such symptoms strongly contribute to the poor functional outcome of some individuals with schizophrenia. However, there is emerging evidence for the use of cariprazine in the treatment of negative symptoms, with initial evidence showing it to be well tolerated. Common side-effects include mild-to-moderate akathisia and Parkinsonism, but there is limited evidence so far of any metabolic side-effect profile.
In general, the lowest possible dose of a single antipsychotic should be used in the first instance. Combinations of antipsychotics should only be considered if there has been inadequate response to individual antipsychotics including clozapine. Patients prescribed an antipsychotic should have regular evaluation of side-effects (for example, using the Glasgow antipsychotic side-effect scale) and frequent monitoring of physical health parameters including vital signs, ECG, weight, and blood tests (lipids, fasting glucose and HbA1c, WCC, U&E, LFTs, and prolactin). In severe psychosis with agitation in the inpatient setting, a rapid tranquilisation protocol, such as intramuscular olanzapine, lorazepam or combined haloperidol and promethazine, may be needed to reduce acute distress and minimise the risk of harm to self and others.
Psychosocial interventions include the use of cognitive behavioural therapy (CBT)
for psychosis, patient and family psychoeducation, behavioural family therapy and programmes aimed at promoting longerterm recovery, such as the Wellness Recovery Action Plan (WRAP), to name a few.
Programmes to reduce the duration of untreated psychosis (DUP) have demonstrated that earlier detection improves outcomes. Ultimately, schizophrenia is a relapsing and remitting illness and two-thirds of people experiencing a first episode of psychosis will have further episodes. Leucht and colleagues (2012) demonstrated that regular antipsychotic medication is protective against relapse in the short-, medium- and long-term. The risk of relapse and poorer outcomes are greater in those with a longer duration of untreated psychosis, a negative attitude towards treatment, a greater burden of side-effects and residual symptoms after treatment. Long-acting injections are a good option for those with frequent relapses due to non- or partialadherence to oral medication. Ultimately, with the correct tools and approach, it is realistic for an individual with schizophrenia to live a pleasurable and meaningful life.
So what happens to Johnny?
He is admitted voluntarily to his local psychiatric unit and assessed by the admitting doctor who recommends commencing a secondgeneration antipsychotic. Johnny is initially reluctant and appears sceptical, but soon begins to trust his treating team and ultimately takes the medication. His symptoms improve and he is offered CBT for psychosis, where he is gently challenged in relation to the delusional beliefs he has in relation to his colleagues. He attends occupational therapy, while family meetings allow for a well-rounded understanding of the challenges he encounters. Following a period of assessment, he is diagnosed with schizophrenia using the criteria outlined of ICD-10. He is discharged home after six weeks and regularly attends outpatient clinics for review. He also attends CBT on an outpatient basis. After a few months, he returns to work on a phased basis and reports feeling more comfortable around other people. He plans to commence a master’s degree next year. ■
References on request
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 12
Progressive supranuclear palsy: An update
Progressive supranuclear palsy (PSP) is a progressive neurodegenerative condition characterised by axial rigidity, oculomotor abnormalities, and cognitive impairment with prominent postural instability and early falls. Pathologically, PSP is characterised by aggregations of tau within the brain. New diagnostic criteria and treatment guidelines have been developed in recent years, which have altered our understanding of PSP. There is no disease-modifying treatment for PSP currently although several agents are under investigation.
Epidemiology and aetiology of PSP
The mean age of onset of PSP is 63 years and progresses to death over approximately seven years, although some subtypes follow a slower course. Estimates of PSP prevalence vary considerably with rates of 5-6 per 100,000 commonly quoted. Estimates of the annual incidence of PSP range from 0.9-1.9 per 100,000.
PSP is typically a sporadic disorder, however, familial cases related to mutations in the MAPT gene as well as a handful of cases related to LRRK2 mutations have been identified, while genome-wide association studies have identified several risk loci of PSP.
Environmental risk factors have been identified related to geographic clusters of PSP. A PSP-like Parkinsonism identified in Guadeloupe has been associated with mitochondrial toxins in annonaceae fruit, while a high rate in an industrial region of northern France appears to relate to exposures to industrial metals.
Other potential risk factors include hypertension, lower levels of education, and rural living. The pathological hallmarks of PSP are microtubule-associated protein tau
aggregates affecting the brainstem and basal ganglia, spreading rostrally to involve the frontal and occipital lobes, and caudally to involve the dentate nucleus and cerebellum. These aggregates are composed of tau isoforms with four microtubule-binding repeats (4R-tau) in the form of neurofibrillary tangles, oligodendrocytic coils, and astrocytic tufts.
Clinical presentation
In their original 1964 paper, Richardson, Steele, and Olszewski described a syndrome of axial rigidity, oculomotor abnormalities, and cognitive impairment. While this so-called Richardson’s syndrome (RS) is the presentation most characteristic of PSP, a much wider range of presentations have been recognised. These variants include Parkinsonism (PSP-P), primary apraxia of gait (PSP-PAGF), corticobasal syndrome (PSP-CBS) and speech and language disturbance (PSP-SL). The 2017 MDS criteria for the diagnosis of PSP recognises eight distinct PSP phenotypes.
Gait and balance impairment are early, disabling, and dangerous symptoms in PSP. Typically, postural reflexes are markedly impaired and patients tend to fall backwards. People with PSP have a stiff, broad-based gait, with knees and trunk extended and arms slightly abducted (sometimes called a ‘gunslinger’ gait) while neck dystonia often produces retrocollis. Patients may pivot wildly when turning due to impaired insight and impulsivity.
Oculomotor abnormalities are a hallmark of PSP. Impairments of vertical saccades are an early finding with downgaze more prominently affected. Other findings include square-wave jerks (saccadic movements with occur during fixation), loss of convergence, and blepharospasm may be seen. Light
sensitivity is common and tinted glasses may help. An inability to look down can cause difficulty reading, walking, and eating (resulting in the ‘messy tie sign’).
Signs evident in the face may include reduced blink rate, frontalis overactivity, and vertical wrinkling of the forehead (the procerus sign) resulting in a troubled or surprised expression. Patients may have difficulty opening their eyes due to dystonia of the tarsal muscles (the common description, ‘apraxia of eyelid opening’, is a misnomer).
The speech disturbance of PSP is characterised by slow, effortful, and distorted speech sometimes referred to as ‘growling’ or ‘gravelly’, which is distinct from both the quiet, monotonous speech of idiopathic Parkinson’s disease (IPD) and the high-pitched, breathy voice of multiple system atrophy (MSA). Language impairment including non-fluent/ agrammatic progressive aphasia and apraxia of speech may be present.
Cognitive impairment in PSP is characterised by frontal lobe dysfunction. Impaired executive function with reduced speed of processing and mental agility, apathy, and spontaneous motor behaviours, such as palilalia and punding may occur. Impulsivity may result in patients attempting tasks they are unable to complete safely. Sleep disturbance is common in PSP with patients frequently describing difficulty initiating and maintaining sleep. REM-sleep behaviour disorder may occur, but is less frequent than in α-synucleinopathies.
Ancillary investigations
A diagnosis of PSP is made on clinical grounds; however, brain imaging can play a supportive role. Classically, brain MRI
13 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
AUTHORS: Dr Shane Lyons1, Dr Sean O’Dowd1, and Prof Tim Lynch 2
1. Neurology Department, Tallaght University Hospital, and 2. Dublin Neurological Institute, Mater Misericordiae University Hospital
demonstrates atrophy of the brainstem, particularly the midbrain. The ratio of pons to midbrain diameter is useful to differentiate PSP from other Parkinsonian disorders. The ‘hummingbird’ and ‘morning glory’ signs, on midsagittal and axial images, respectively, are seen in PSP, but lack sensitivity. The magnetic resonance Parkinsonism index (MRPI) is calculated by multiplying the pons areamidbrain area ratio (P/M) by middle cerebellar peduncle (MCP) width-superior cerebellar peduncle (SCP) width ratio (MCP/SCP) and helps to identify cases of Parkinsonism likely to evolve to PSP. PET imaging reveals decreased glucose metabolism in the midbrain early in the disease course while decreased metabolic activity in the caudate, putamen, and prefrontal cortex occur later. New PET imaging modalities using ligand which bind to the tau protein may enable earlier diagnosis or more accurate measurements of the progress of disease.
Treatment
A range of strategies are used to ameliorate symptoms and improve quality-of-life in PSP. Few randomised control trials exist in PSP, and treatment strategies are largely based on clinical experience and observational studies. In 2021 the CurePSP Centres of Care Network published a consensus statement on the management of PSP which provides helpful guidance on a range of treatment modalities (available here: www.frontiersin.org/ articles/10.3389/fneur.2021.694872/full).
The involvement of a multidisciplinary team (MDT) with experience in neurodegenerative disease is essential in treating PSP. Physiotherapy can be useful to maintain strength and improve balance and coordination. The selection of appropriate walking aids is important. Lightweight wheelchairs with a tilting mechanism to prevent falling out are preferred. Occupational therapy intervention for functional and domestic adaptation is helpful. Speech therapy support for communication including the use of alphabet boards, text-tospeech systems, and repetitive exercises play a role. SLT also provide important support for swallowing difficulties.
Appointing an enduring power of attorney
early in the disease course can simplify later decisions. The social and caring challenges are significant. Support from a range of sources including the hospital team, community services, and patient organisations such as the Progressive Supranuclear Palsy Association (PSPA) is essential. Early involvement of palliative care in the MDT can be extremely helpful, especially with regard to the need for hospice care as well as the management of multiple complex symptoms.
Important pharmacological options to consider in PSP include:
Levodopa may help with bradykinesia, rigidity, and tremor: 20-to-30 per cent of patients with PSP respond to levodopa. A target dose of 800-1200mg per day is usually recommended.
Amantadine, titrated to a maximum dose of 100mg tds, may be helpful for gait dysfunction but may have deleterious cognitive effects.
Liposomal coenzyme Q10 (100mg tds) provides a benefit to gait in a small proportion of patients and a trial is recommended.
Baclofen and benzodiazepines may be helpful for dystonia.
Melatonin can be useful for insomnia.
Cholinesterase inhibitors should be used only where there are pronounced amnestic deficits and otherwise are best avoided.
Botulinum toxin may be helpful for focal dystonia and for apraxia of eyelid opening, while injection of the parotid glands can be helpful for the control of sialorrhea.
Although no treatment currently exists to slow or arrest the course of PSP, a number of potential therapies are under investigation. Disappointingly, 2021 saw negative results for two trials of anti-tau monoclonal antibodies directed against the N-terminal of tau (gosuranemab and tilavonemab), however, further studies are ongoing, including monoclonal antibodies targeting alternative binding sites on the tau protein (UCB0107), agents which modify mitochondrial function (MP201) or lipid peroxidation (RT001), and antisense oligonucleotides to reduce the production of tau (NIO752).
A persistent challenge in trials of PSP, as in all neurodegenerative disease, is that by the
time a diagnosis is made with confidence significant neurodegeneration has occurred and prospects of effective treatment are diminished. The search for early and reliable biomarkers, either imaging or CSF-based, may allow early identification of cases and initiation of treatment at an earlier stage.
PSP care and research in Ireland
To tackle the lack of epidemiological data on PSP in Ireland an Irish multicentre epidemiological study, ‘The Leinster Tauopathy Study,’ is in preparation and hopes to begin recruiting participants in early 2022. The study brings together Irish expertise in atypical Parkinsonism from Dublin hospitals and will seek referrals of patients with a possible diagnosis of PSP or CBS and a home address in Leinster. The study aims to establish the prevalence and incidence of PSP and CBS in an Irish population and plans to establish a biobank of blood, DNA, and cerebrospinal fluid samples to facilitate future studies of diagnostic and prognostic biomarkers. Developing an accurate picture of the population with tauopathies and their needs will help to inform future service provision. Also this month (January 2022), Tallaght University Hospital will become accredited as the only Irish site in the European Research Network for Rare Neurological Diseases (ERN-RND) as an expert centre for atypical Parkinsonism. This prestigious designation will allow patients to access a broader range of specialist expertise.
Conclusion
PSP is a complex, progressive, neurodegenerative condition which has an enormous impact on the daily functioning, quality-of-life, and social circumstances of patients and their families. Patients commonly present with axial rigidity, gaze abnormalities, and cognitive impairment, although a wide range of phenotypes are described. Although no disease-modifying treatment exists, a range of therapies may help manage the symptoms and complications of the condition. In Ireland we are developing services for patients with PSP and other atypical Parkinsonian disorders, as well as national and international research projects and collaborations.
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 14
The common manifestations of anxiety disorders
AUTHORS: Dr Niall Duffy, Registrar in Psychiatry, Cluain Mhuire Service, Blackrock, Co Dublin; and Dr Stephen McWilliams, Clinical Associate Professor, School of Medicine, University College Dublin, and Consultant Psychiatrist, St John of God Hospital, Stillorgan, Co Dublin
CASE REPORT
Chloe is a 19-year-old female who presents to the emergency department (ED) stating that she feels like she is having a heart attack. A first-year student at a local university, she attended a class in a crowded lecture theatre earlier today and describes having felt nervous on arrival as she couldn’t find a seat near the back of the hall. Chloe’s friend is enrolled in the same course as her, but was off sick today. Chloe reports that she suddenly started shaking, experienced her heart racing, and became short of breath before developing pains in her chest. She describes feeling terrified, as though she was “going to die”. She recounts being escorted out of the lecture hall by a classmate and now feels embarrassed that such an incident happened in front of so many people. She is seen by the SHO in the ED, and has routine blood tests, a physical examination and an ECG, all of which prove normal. Chloe is discharged from the ED, only to return three days later with a similar presentation. She is tearful and expresses uncertainty regarding her future. This time, she is referred to the liaison psychiatry service for further assessment.
The American Psychological Association defines anxiety as “an emotion characterised by feelings of tension, worried thoughts and physical changes”, such as sweating, palpitations, dizziness, and shaking. All of us experience at least some anxiety in our lives, but clinically-significant anxiety that crosses the door of a GP surgery or psychiatric clinic must be severe enough to affect our everyday functioning and cause significant distress.
Anxiety disorders are common worldwide. A systematic review published in Brain and Behaviour in 2016 – well before the Covid-19 pandemic – demonstrated the prevalence of anxiety disorders to range from 4-to-25 per cent with higher rates in females, younger adults, those with chronic diseases and Euro/ Anglo subgroups. Anecdotally, we have seen patients presenting more frequently with anxiety symptoms to our hospital and outpatient clinics during the Covid-19 pandemic, with early data showing that more than one-in-four adults living in the Republic of Ireland screened positive for generalised anxiety disorder or depression during the initial lockdown of March 2020. Such figures have been replicated in the UK.
Anxiety disorders are diagnosed using the World Health Organisation’s International Classification of Diseases (ICD-10/ICD-11) or the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The year 2022 will see the adoption of the ICD-11, with the now-out-ofdate chapter on ‘Neurotic, stress-related and somatoform disorders’ in the ICD-10 replaced by four groupings, namely:
1. Anxiety and fear-related disorders;
2. Obsessive-compulsive and related disorders;
3. Disorders specifically associated with stress; and
4. Dissociative disorders.
This article will focus on the ICD-11 disorder grouping of ‘anxiety and fear-related disorders’.
Generalised anxiety disorder (GAD) is the first disorder in this group. It is characterised by marked anxiety symptoms that are present on most days over a period of several months. It manifests as either free floating anxiety,
such as a consistent feeling of apprehension, or an excessive worry about normal everyday events. The individual can present as restless or irritable, with poor concentration, disrupted sleep and autonomic arousal leading to, for example, palpitations, nausea and hyperventilation. Screening tools such as the Generalised Anxiety Disorder Assessment (GAD-7) can be helpful both in hospitals and primary care settings to establish the severity of anxiety symptoms over the previous two weeks.
The second disorder in this group is panic disorder which consists of recurrent panic attacks, namely intense, rapid-onset periods of extreme worry and physical symptoms such as palpitations, sweating, chest pain, shortness of breath, dizziness. An intense fear of imminent death can occur, while the individual may be preoccupied with the return of a panic attack and thus engage in avoidant behaviours to prevent further attacks.
Agoraphobia involves intense fear or anxiety when an individual is faced with a situation from which they perceive escape to be difficult. Common examples include crowded places away from home such as a busy shop, a marketplace, or public transport. Avoidance of these situations for fear of embarrassment is a prominent feature. Agoraphobia can present with the physical symptoms of panic disorder as outlined above.
Specific phobias include arachnophobia (fear of spiders), acrophobia (fear of heights), and claustrophobia (fear of confined spaces). They present with severe anxiety and fear when the individual is exposed to (or anticipates exposure to) the particular phobic object or situation. Such fear is significantly out of proportion to the actual risk or danger, and the individual avoids the object or situation wherever possible.
15 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
With social anxiety disorder, an individual experiences marked symptoms of anxiety and distress in one or more specific social circumstances. Some social situations are typically avoided (eg, giving a presentation to peers or eating in public) as the individual fears that they will be perceived in a negative way by others.
The final two disorders in this grouping are separation anxiety disorder and selective mutism. These disorders were originally placed in the childhood disorders chapter of the ICD-10. When an adult develops separation anxiety, it is usually related to an ‘attachment figure’, such as a partner, spouse or child. The individual can experience marked distress when separated, with recurrent nightmares and a refusal to sleep away from the attachment figure. The symptoms must be present for at least several months before a diagnosis can be made. Selective mutism more commonly occurs in children, and typically presents with selectivity in speech in certain social situations such as school. Symptoms must be present for at least one month before a diagnosis can be considered.
For the diagnosis of an anxiety and fearrelated disorder, the symptoms cannot be a direct result of drugs or medications which have effects on the central nervous system. The symptoms must be severe enough to cause significant distress, along with functional impairment in the individual’s life. Depression, alcohol misuse, and drug abuse are common comorbid conditions seen with anxiety disorders which, if left untreated, can aggravate the course and worsen the prognosis.
Treatment
The overall goal in treating anxiety disorders is symptomatic relief, functional improvement and a reduced risk of relapse. The UK’s National Institute for Health and Care Excellence (NICE) has published clear guidance using a ‘stepped care’ approach. The earlier steps predominantly focus on psychological interventions, with individual self-help, psycho-education groups, and cognitive behavioural therapy (CBT) as recognised first-line treatments. Individuals with marked functional impairment, or those who don’t respond to psychological
approaches, will ultimately require pharmacological intervention.
In GAD, the NICE guidance advises sertraline first as it is most cost-effective. If this is ineffective or not tolerated, another SSRI, or an SNRI such as venlafaxine, should be offered. Similarly, for panic disorder, social phobia and agoraphobia, SSRIs should be used as first-line options. Benzodiazepines should not be offered except on a short-term basis during periods of crisis, the exception being panic disorder where they should not be used at all. Pregabalin is listed as a later option in the Maudsley Prescribing Guidelines for treatment of GAD and social phobia; however, it should be used with caution given emerging evidence of its potential for addiction. It is best avoided if there is a history of drug misuse in the patient’s past.
If there is concern about a patient’s risk or, indeed, inadequate response to psychological and pharmacological interventions, a referral to a specialist mental health service should be considered. Here, a combination of biological and psychological approaches can be used, with access to a multidisciplinary team, a day hospital, a crisis centre and an inpatient unit. Exercise, mindfulness, relaxation and breathing techniques are all recognised adjuncts to the psychological and pharmacological management of anxiety. Results from the Irish longitudinal study on ageing show that high volumes of physical activity are associated with lower anxiety symptoms.
Although we witnessed an increase in anxiety and depressive symptoms in the general population in the early stages of the Covid-19 pandemic, research shows that the prevalence of mental health symptoms returned to pre-pandemic levels by summer 2020. It remains to be seen whether the pandemic has had a significant, longer-term impact on the prevalence of anxiety disorders in our population.
So what happens to our care report patient?
Chloe is seen and assessed by her local community mental health service. On further exploration of her symptoms, she reports a history of anxiety symptoms dating back to
her adolescent years. Her main difficulties occur when out in public, with marked physical symptoms of anxiety while in her local shopping centre. As a result, Chloe tends to avoid going to these places alone; she will only go with her mother or friend. Indeed, she usually does her shopping online. She is ultimately diagnosed with agoraphobia with associated panic attacks, and is prescribed sertraline. Chloe is referred for CBT with a focus on graded exposure (developing an exposure-fear hierarchy) with gradual progression to situations that tend to cause the most severe anxiety symptoms. Chloe engages well in CBT and makes excellent progress. She continues to be followed up regularly by the community mental health team for medication management and mental state assessment.
References
1. Taylor D, Barnes T, Young A. The Maudsley Prescribing Guidelines in Psychiatry – 13th Edition
2. World Health Organisation. The ICD-11 Classification of Mental and Behavioural Disorders. Available at: https://icd.who.int/en
3. Reed G, et al. Innovations and changes in the ICD-11 Classification of Mental, Behavioural and Neurodevelopmental Disorders. World Psychiatry 2019; 18:3-19
4. National Institute for Health and Care Excellence. Generalised anxiety disorder and panic disorder in adults: Management. Clinical Guideline 113, 2011. Available at: www.nice.org.uk/guidance/cg113
5. Hyland P, et al. Anxiety and depression in the Republic of Ireland during the Covid-19 pandemic. Acta Psychiatrica Scandinavica 2020: 142: 249-256
6. Hyland P, et al. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the Covid-19 pandemic. Psychiatry Research 300 (2021) 113905
7. Remes O, et al. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain and Behaviour, 2016: 6(7), e00497
8. McDowell CP, et al. Associations of physical activity with anxiety symptoms and status: Results from the Irish Longitudinal Study on Ageing. Epidemiology and Psychiatric Sciences (2019), 28, 436-445
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 16
Tallaght University Hospital and CHI join European network of expert centres for rare neurological diseases
AUTHORS: Shane Lyons1, Sinead Murphy1, Richard Walsh, Sean O’Dowd1 1Neurology Department, Tallaght University Hospital, Dublin 24
The neurology service at Tallaght University Hospital (TUH) provides a comprehensive service to patients with neurological diseases to a catchment population of 450,000 people. The department provides a range of subspecialty services including clinics for movement disorders, inherited neuropathies, neuromuscular diseases, cognitive disorders, neuroinflammatory disorders, headache, vascular neurology, and the National Ataxia Clinic. From January 2022, the neurology service at TUH will become an expert centre for both atypical Parkinsonism and cerebellar ataxias and hereditary spastic paraplegias within the European Reference Network for Rare Neurological Diseases (ERN-RND). The expert centre designation for cerebellar ataxias and hereditary spastic paraplegias is in conjunction with paediatric colleagues in Children’s Health Ireland (CHI) based at both TUH and Temple Street. This exciting new development in neurological care will improve patient access to European expertise in these rare neurological diseases while fostering links with other expert centres and helping to develop services for RNDs in Ireland.
RNDs in Europe (and beyond)
The European Union (EU) considers a disease to be rare when it affects fewer than one in 2,000 people. While each individual rare disease affects only a small number of people, there are over 6,000 rare diseases with the result that rare diseases as a group affect an estimated 30 million Europeans. Many rare diseases are associated with neurological symptoms affecting the central nervous system, peripheral nerves, or muscle. Well-known rare neurological diseases
include Huntington’s disease, Duchenne’s muscular dystrophy, and progressive supranuclear palsy but many others are little known and often evade diagnosis. The low prevalence of individual diseases means that no single centre, or even single country, can have expertise in all rare diseases. Therefore, patients with rare conditions, and their families, often face barriers to diagnosis and treatment due to lack of available expertise. This ‘diagnostic odyssey’ may involve visits to multiple physicians and (particularly in small island nations like Ireland) international journeys to specialist centres. This is a particular challenge in neurological disease where early diagnosis may be key to accessing clinical trials or emerging novel therapeutics to reduce disability. This is likely to become more important in the near future as diseasemodifying therapies become available. Rare neurological diseases include many genetic disorders and also conditions caused by the spread of abnormal proteins within the brain (proteinopathies).
Patients may soon be able to benefit from new advances such as viral vector-based gene therapy, antisense oligonucleotides, and monoclonal antibodies targeted at abnormal proteins.
European Reference Networks
In 2017 a number of ERNs were launched, connecting more than 900 healthcare units across 26 countries within the EU to improve access to expertise in rare, complex diseases for European patients. The central goal of the ERNs is to use telemedicine to allow medical expertise to travel rather than the patient. Bringing expertise to the patient in this manner can improve healthcare quality, reduce
inequalities of access, and increase medical expertise across the EU. The ERN-RND is the network which deals with rare neurological disease. The ERNRND includes six sub-themes including ataxias, chorea, frontotemporal dementia, leukoencephalopathies, dystonia, and atypical Parkinsonism. The network includes 32 centres and, as outlined, will expand to include TUH and CHI within the cerebellar ataxias and hereditary spastic paraplegias and atypical Parkinsonism syndromes subgroups in 2022.
A key aim of the ERN-RND is to increase the percentage of patients with RND who receive a confirmed molecular diagnosis. Patients in whom a diagnosis has not been successfully made can be discussed by an expert panel using the Clinical Patient Management System (a web-based clinical software application which allows secure remote case discussions). Healthcare professionals within the ERN can upload patient data to this system to seek input for experts throughout the network.
Conclusion
This year will see a significant advance for neurology in TUH and CHI as together the services join the ERN-RND. This development will give Irish patients with RND access to a broad range of clinical knowledge from all over the EU. At the same time physicians at TUH and CHI will be able to contribute Irish expertise and experience to our European colleagues.
More information on the ERNs is available on the website of the European Commission, https://ec.europa.eu/health/ern/ networks_en. For more details on the RND network please see www.ern-rnd.eu
17 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
Diagnosis and treatment of bipolar affective disorder
AUTHORS: Dr Niall Duffy, Registrar in Psychiatry, Saint John of God Hospital, Stillorgan, Co Dublin; and Dr Stephen McWilliams, Associate Clinical Professor, School of Medicine and Medical Sciences, University College Dublin, and Consultant Psychiatrist, Saint John of God Hospital, Stillorgan
CASE REPORT
Jane is a 28-year-old female brought to the emergency department by her mother, who is concerned that Jane has not been sleeping for the last week. On assessment Jane tells you that she has a lot of ideas and plans about how she can cure Covid-19, showing you a notebook of nonsensical words and symbols. She reports having a lot of energy, and doesn’t feel the need to sleep. Her speech is loud and rapid and she often jumps from one topic to the next. She only agreed to come to hospital in order to pitch her ideas and can’t understand why she isn’t meeting the head of department. She is quite dismissive of you and has difficulty in sitting still during the assessment.
Bipolar affective disorder is a common psychiatric illness which holds a lifetime risk of around 1 per cent, affecting both men and women equally. The first episode most commonly occurs between the ages of 15 to 30 years, but may occur at any age.
Bipolar disorder can be diagnosed in accordance with the ICD-10 Classification of Mental and Behavioural Disorders when there have been at least two episodes of significant disturbance in a person’s mood and activity levels. The disturbance in some occasions will be mania or hypomania (mood elevation, an increase in energy and activity) and in others of depression (lowered mood, a decrease in energy and activity).
Hypomania is classified as an abnormality of mood and behaviour which is outside of the normal for the individual, but not to the extent that it leads to severe or complete disruption in work or function. Elevated and irritable mood lasts for at least four days, with a minimum of three additional symptoms including a decreased need for sleep, irritability, increased activity, overfamiliarity, reduced concentration and reckless behaviour like overspending.
In mania, mood elevation remains out of keeping from the individual’s normal character and is more severe. It differs from hypomania by lasting for at least one week, and should be significant enough to disrupt ordinary work and social activities more or less completely. Mood change should be accompanied by increased energy, and several of the other symptoms listed above including grandiosity, pressure of speech and decreased need for sleep. Psychotic symptoms such as grandiose or religious delusions of identity or role, hallucinations and thought disorder can feature in around 20 per cent of patients. Severe and sustained physical activity and excitement can result in physical neglect.
For an episode of depression, the person may report a lowering of mood, loss of enjoyment and reduced energy levels leading to a reduction in activity. There are numerous other common symptoms including disturbed sleep (difficulty in falling asleep, or early morning awakening), reduced appetite, poor concentration, feeling hopeless, worthless or guilty, reduced self-esteem, thoughts of self-harm or suicidal ideation. Episodes can be classed as mild, moderate or severe, depending on the amount of symptoms the individual experiences. For an episode of depression to be diagnosed, symptoms must be present for
at least two weeks. Mood may be worse at a certain time of the day, however, there tends to be little variation in mood from day to day.
Manic episodes tend to start abruptly, and may last for up to four-to-five months. Depressive episodes can last longer with a more gradual onset. Mood disturbances often follow stressful life events, but that is not essential for diagnosis. In most circumstances there is complete recovery between episodes of mood disturbance.
ICD-11, which is due to be adopted formally in 2022, will subdivide ICD-10’s definition of bipolar affective disorder into bipolar Type I and bipolar Type II, following a similar pattern to DSM-5. Bipolar Type I involves alternating episodes of depression with manic episodes, whereas bipolar Type II involves alternating episodes of depression with hypomanic episodes. Rapid cycling bipolar disorder is characterised by at least four episodes of mood disturbance within the same year.
Research into the aetiology of bipolar disorder is ongoing. The causes are believed to be multi-factorial in nature. Genetics are thought to be important with twin, family, and adoption studies all showing significant familial contribution. First-degree relatives of someone with bipolar disorder are more likely to develop the illness in comparison to the general public. Certain environmental factors including stressful life events, pregnancy, and sleep disturbance can play a role.
Treatment
Treatment follows a typical biopsychosocial approach and admission is recommended in more severe cases of mood disturbance as a safer way to assess and manage symptoms.
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 18
Antidepressant medications should be stopped in cases of mood elation, with patients typically commenced on an anti-manic agent. The Maudsley Prescribing Guidelines recommend an antipsychotic, lithium or valproate as first-line based on available research. Cipriani et al compared the efficacy of a number of different anti-manic agents, finding that overall olanzapine, haloperidol and risperidone were the best available at treating acute mania. In addition lithium, valproate, carbamazepine, and other antipsychotics, such as quetiapine, aripiprazole, and ziprasidone were significantly better than placebo at treating acute mania. In practice, antipsychotics tend to be used first in the treatment of acute mania as mood stabilisers, such as lithium, are limited by the fact that it usually takes around a week to achieve a response.
Episodes of bipolar depression, when compared to unipolar depression, tend to be more rapid in onset, more severe and more frequent. If a person develops a moderate to severe episode of bipolar depression, the National Institute for Health and Care Excellence (NICE) in the UK recommend either quetiapine or a combination of fluoxetine and olanzapine. If they fail to respond, lamotrigine should be offered. There is less available evidence for treating bipolar depression than mania, and the use of antidepressants may increase the risk of precipitating a manic episode. Treatment should be at the level of secondary care.
For longer-term treatment of bipolar disorder, lithium is normally recommended as the first-line agent to prevent relapse of mood disturbances. It is better at preventing manic than depressive relapses, and response will likely be better the earlier lithium is commenced. Lithium is renally excreted, and has a narrow therapeutic index for treatment response. The optimal range is between 0.6-0.75mmol/L and levels below 0.4mmol/L are likely to be ineffective. Baseline renal and thyroid function tests in addition to a full blood count, calcium, ECG and calculation of BMI are recommended prior to commencement.
A 12-hour post-dose serum lithium level should be checked every five-to-seven days until a steady state is reached.
Most side-effects are dose related and typically include dry mouth, a metallic taste, fine tremor, polyuria, weight gain and aggravation of skin conditions. In the longer term, lithium can result in a reduction in renal function, and increases the risk of hypothyroidism therefore warranting the monitoring of serum lithium level, renal function and thyroid function every three-to-six months.
Serum lithium levels of greater than 1.5mmol/L can result in lithium toxicity which may present with vomiting, coarse tremor, ataxia, nystagmus, confusion, and impaired consciousness. Due to the narrow therapeutic index, some drugs such as ACE inhibitors, NSAIDs and diuretics can precipitate toxicity.
Pregnancy is a relative contraindication to lithium, given the 20-fold increased risk of Ebstein’s anomaly, a congenital heart defect.
A systematic review by Hui et al published in 2019 highlighted a number of predictors of good response to lithium including shorter pre-lithium illness duration, family history of bipolar disorder, older age of onset, absence of rapid cycling and an absence of psychotic symptoms. Evidence shows that lithium also offers some protection in both attempted and completed suicide in patients with bipolar illness.
Valproate is another commonly used mood stabiliser, however NICE recommends that it should not be used in women of childbearing age due to teratogenicity risk. Valproate should only be considered if other options are ineffective and a pregnancy prevention programme is in place. Common side-effects include nausea, lethargy, weight gain, gastric irritation, sedation, and in some cases hair loss, thrombocytopaenia, and hepatic failure. Carbamazepine and lamotrigine are also best avoided in pregnancy because of teratogenic risk.
Structured psychological approaches, such as cognitive behavioural therapy (CBT), and
psychosocial interventions for patients and family, such as the ‘Wellness Recovery Action Plan’ should be offered with an emphasis on education and relapse prevention methods.
Relapse and remission rates vary among literature, but positive prognostic factors include periods of shorter duration of illness, few psychotic symptoms, few comorbid physical problems, and of course good treatment response and adherence to treatment plan.
So what happened to Jane?
She was admitted to her local psychiatric unit and commenced on olanzapine for mania, and benzodiazepines short-term to reduce distress. She had frequent reviews by the multidisciplinary team (MDT), which included CBT and family psychoeducation on bipolar disorder. Prior to discharge she was commenced on lithium for prophylaxis of further mood episodes and will be followed up by the community mental health team. ■
References
1. The International Classification of Diseases (ICD-10), World Health Organisation, 1993
2. The Diagnostic and Statistical Manual (DSM-5), American Psychiatric Association, 2013
3. Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines in Psychiatry, 12th Edition, 2015
4. Semple D, Smyth R. Oxford Handbook of Psychiatry, Third Edition, 2013
5. National Institute for Health and Care Excellence. Bipolar Disorder: The assessment and management of bipolar disorder in adults, children and young people in primary and secondary care. Clinical Guideline 185, 2014
6. Cipriani A, Barbui C, Salanti G, et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta analysis. Lancet, 2011: 378 (9799):1306-15
7. Hui TP, Kandola A, Shen L, et al. A systematic review and meta-analysis of clinical predictors of lithium response in bipolar disorder. Acta Psychiatrica Scandinavica 2019: 140: 94-115
19 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
Migraine: Medication overuse and medication-overuse headache
Headache is a very common complaint in primary care, accounting for up to 5 per cent of all general practice consultations. Most patients attending doctors suffer from primary headache disorders, predominantly migraine (more than 90 per cent).
Migraine is often treated with painkillers or acute medications. In fact, this is the most common reason for analgesic use in the general population. Many migraine patients unfortunately acquire the additional complication of medication overuse (MO), which can in turn lead to medication-overuse headache (MOH). Migraine patients who have MO and/or MOH are often very debilitated and this group of conditions together are a substantial burden on society.
During our undergraduate training we all received training about the headache that is associated with a potentially sinister or lifethreatening secondary headache condition, for example, sub-arachnoid haemorrhage (SAH). GPs see three-to-four people with SAH during their medical lifetime. To date, there has been little emphasis on MO and MOH in the undergraduate medical curriculum, despite the latter being more frequent.
MO, MOH, and probable MOH are seen frequently in general practice (and often not diagnosed); 1-to-2 per cent (in developed countries), with a range between 0.5 per cent and 7.2 per cent. The highest prevalence has been shown in Russia (7.2 per cent). The prevalence of MO/MOH in specialist headache clinics in Ireland and internationally ranges from 30-to-50 per cent. ‘Status migrainosus’ is when a debilitating migraine attack lasts longer than 72 hours. It may often be caused by MO.
Medication overuse
MO is formally defined as the use of:
Simple analgesia (such as paracetamol or non-steroidal anti-inflammatories
(NSAIDs)) 15 or more days per month for at least three months; or
Combination analgesics (often codeine/opiate based, such as Solpadine) or triptans 10 or more days a month for at least three months.
It is important to differentiate between the practice of MO (that is, taking painkillers, NSAIDs, triptans or combination products too frequently) and the secondary headache condition, MOH. Determining MO is generally very easy in a cohort of migraine patients as long as a detailed history is taken.
Difficulties encountered in taking a detailed history for MO
In general practice, some patients may be impatient and unwilling to give a detailed history as typically their primary goal is to get a ‘quick fix’ for the pain and the other disabling symptoms. In addition, general practice is usually very busy and the standard consultation time is insufficient (10-to-15 minutes). Furthermore, in our clinical experience:
Some patients are poor historians and are more resistant to history taking and giving exact details of how much medication they are taking;
Patients with MO (and MOH) are typically more resistant to repeated questioning and may be more defensive;
Patients do not usually volunteer information on how much acute medication they are taking as they may be trying to hide it;
Many of them do not understand that it is related to the worsening of their headaches.
Together, these multiple issues often result in an unsatisfactory consultation, and contribute to under-diagnosis and under-treatment of MO, MOH, and probable MOH. Therefore, a complete list of all non-prescribed and prescribed medications should be obtained with a view to assessing if the patient has MO or more rarely, MOH in those who have
headaches. In clinical practice, we have found that many headache/migraine patients may need to be interviewed several times about their symptoms and medication intake, often on separate occasions. For some patients, this may feel like an interrogation. However, the healthcare professional has an obligation to ask probing questions in order to do everything possible to get the correct diagnosis, so that they can treat the patient appropriately. The key factor for defining MO is the number of days per month that acute medication is taken for headache. It does not appear to be relevant in this context whether a single dose or multiple doses of the acute headache medication are used on a particular day.
In our clinical practice, we generally advise our headache patients that analgesics or acute medication should be used no more than fourto-six days per month (see Table 1), in order to avoid MO. The overuse of medication typically begins with patients taking over-the-counter (OTC) painkillers more regularly, and this often starts well before the patient consults with their GP. When the practice of MO leads to a change in headache pattern and resistance to conventional migraine prophylactic treatment, the patient is then described as having MOH or probable MOH.
MO – When is it time for prophylactic migraine treatment?
MO in the context of more chronic migraine is a worldwide public health problem. Despite repeated public awareness campaigns nationally and internationally over the last two decades, this issue is still a significant cause of disability in a large proportion of high-frequency episodic and chronic migraine patients.
As a general guideline, preventive or prophylactic therapy is indicated in patients with migraine who have headache and associated neurological symptoms:
On eight-to-10 days per month or
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 20
AUTHOR: Dr Mary Kearney, GP with extended role in headache, Tutor at the ICGP
more (usually for a period of at least three-to-six months);
And have at least moderate disability due to their headache attacks.
In other words, the key factors in decision making are the number of days per month that patients experience symptoms, together with the level of disability in each individual migraine patient. An additional aim of preventive therapy is to try to treat moderateand high-frequency episodic migraine effectively before MO develops. It should be emphasised that if there is established MO and chronic migraine, there is strong evidence to suggest that many conventional prophylactic treatments are ineffective or less effective.
A pragmatic individualised approach to preventive therapy needs to be taken with patients who experience intermediatefrequency episodic migraine and associated migraine symptoms between five-to-seven days per month, considering:
The level of disability from migraine attacks;
Efficacy of the prophylactic treatment in each specific individual;
Patient preference; and
Severity of side-effects to a specific preventative therapy should dictate whether or not a patient starts with (or continues on) prophylactic treatment.
We do not feel that it is appropriate to offer medium-term (typically one-to-two
years) conventional daily oral prophylactic medications for migraine to patients with one-to-four migraine or headache days per month. We consider this practice to be somewhat excessive, due to the associated side-effects of daily medications and the lack of overall efficacy of these preventive agents. Patients with low-frequency episodic migraine should be encouraged to treat early with a combination of acute medications.
Strategies for prevention of MO in migraine patients
We recommend an integrated care approach to prevention and management of MO in patients with migraine. This should involve hospitalbased healthcare professionals (neurologists, specialist nurses, psychologists, etc), primary care physicians, pharmacists, general practice nurses, community psychology and psychiatry, and the voluntary patient groups, such as the Migraine Association of Ireland (MAI).
We feel that the following should be considered to try and prevent MO and MOH:
1) Written patient information leaflets/booklets on MO have been developed and should be given to those migraine patients who are potentially at risk of progressing to MO.
2) Pharmacists are ideally placed in primary care to identify patients who may be at risk of MO. Therefore, it is essential to include and collaborate with pharmacists to highlight this message to patients.
3) The value of pharmacy involvement has now been highlighted through their inclusion in the national Sláintecare headache programme.
4) The Migraine Association of Ireland (MAI) also provides written information for patients and has extensive information on their website about MO and MOH.
5) Headache diaries should record which acute medications are used and how frequently. As chronic headaches are assessed over a three-month period, a review of the last three months of the diary is ideal.
6) There should be caution in primary care and emergency departments when prescribing codeine (which is metabolised as an opiate) or opiate-based analgesia, as they are often responsible for MO and there is also the potential for dependence and possibly addiction.
Opiate-based medication may also cause drowsiness, incoordination and possibly impair driving. All patients should be advised of this when they get a prescription. It is generally advised that headache patients should avoid codeine, tramadol, and other opiate derivatives.
Paracetemol Max dose – 4,000mg in 24 hours
Naproxen Max dose –1,000mg in 24 hours
Ibuprofen
Max dose – 2,400mg in 24 hours
Diclofenac Max dose – 150mg in 24 hours
Aspirin Max dose – 4,000mg in 24 hours
Mefanamic acid
Max dose – 1,500mg in 24 hours
Sumatriptan 50-100mg
Max dose –300mg in 24 hours
Zolmitriptan 2.5-5mg daily
Max dose –10mg in 24 hours
Frovatriptan 2.5mg
Max dose –5mg in 24 hours
Naratriptan 2.5mg
Max dose – 5mg in 24 hours
Almotriptan 12.5mg
Max dose – 25mg in 24 hours
Most migraine patients with MO will have been in contact with their GP for their headache. In fact, almost half will have had such a contact in the previous year. The GP, therefore, should have a key role in providing education, advice, and support, in addition to prescribing prophylactic medication where appropriate. This would be particularly true for those with a medical card in Ireland, as most (or all) medications are put on the general medical services (GMS) prescription.
Medication-overuse headache
MOH appears to be almost exclusive to those who suffer from migraine. The term was first used in 2004. Historically, since its initial documentation in the 1950s this type of headache has been called analgesic rebound headache, medication-misuse headache, transformed migraine or druginduced headache. A three-month headache diary may be useful for patients to keep a
21 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
ANALGESIA NSAID s TRIPTANS
MEDICATION FOR ACUTE MIGRAINE ATTACK TO BE USED FOUR-TO-SIX DAYS PER MONTH
TABLE 1: Adopted from How to treat your headache acutely unpublished work (Ruttledge) with permission. Professional version. Patient friendly version also available
detailed record of medication use. The most common medications, most of which have been mentioned previously, are implicated and include:
Simple analgesia (such as paracetamol);
Combinations of paracetamol or ibuprofen with codeine (eg, Neurofen plus or Solpadine);
Paracetamol/tramadol combination;
Triptans (now that sumatriptan is available OTC);
Tapentadol and other opiates.
Patients may substitute one for the other. The perfect example being the reduction in use of codeine since the 2007 Irish (and international) campaign to reduce analgesic use and the concomitant increase in the regular use of triptans and simple analgesia. On a national level, people have become aware that analgesia are available more freely in Northern Ireland (or Spain) without a prescription and tend to get a supply when there.
Determining MO is generally very easy in a cohort of migraine patients as long as a detailed history is taken. However, diagnosing MOH is a more difficult task. There is even confusion in the international literature regarding the description and definition of these two related concepts. In recent years, experts speaking on this topic at headache/ migraine conferences are usually at pains to define each entity carefully. Management of these patients is also a controversial topic at many of these meetings.
CRITERIA FOR DIAGNOSIS OF
HEADACHE
A. Headache occurring on >15 days/ month in a patient with pre-existing headache disorder; and
B. Regular intake of paracetamol or one or more NSAIDs on >15days/month for more than three months; and/or
C. Regular intake of one or more opioids/ codeine* on >10 days/month for more than three months; and/or
D. Regular intake of one or more triptans >10 days/month for more than three months
A recent retrospective study from a specialist clinic in Buenos Aires in 2019 documented MO in slightly more than 40 per cent of their chronic migraine patients attending the clinic. The study also concluded that migraine is the most frequent primary headache, closely followed by the secondary condition MOH. It is important for GPs to consider these problems and identify patients who are overusing acute treatments and also patients with MOH. These individuals are more likely to experience more chronic and disabling headaches, which are very difficult to manage unless the diagnosis of MO and MOH is considered and subsequently addressed.
How the cycle of MOH starts
For the sake of clarity, MOH is defined as headache worsening by the practice of MO and is almost always seen in patients with migraine biology. To make the diagnosis of MOH, the headache disorder must become more frequent and chronic. It is recognised as a separate secondary headache disorder in the third and most recent version of the International Classification of Headache Disorders (ICHD-3)
The biological basis of MOH is a topic of international debate and is not clearly understood. In practice, MOH (or probable MOH) develops as a secondary headache disorder following on from MO, in circumstances where the headache frequency increases and this results in increasing acute medication or painkiller use. MOH is then deemed to be clinically evident when there is
clear chronification of the headache disorder and concomitant resistance to conventional pharmacological prophylaxis. The overuse behaviour can happen almost without the doctor or the patient realising it is a significant problem.
The diagnosis of MOH is supported if the headache frequency is reduced on withdrawing the offending acute medication. In specific individuals, MOH may be encouraged further as a result of using less effective or non-specific acute medications, resulting in inadequate treatment response and re-dosing. For example, a less effective strategy might be to take paracetamol or ibuprofen alone, rather than a more effective combination approach of paracetamol, ibuprofen and a triptan together at the same time (see Table 1).
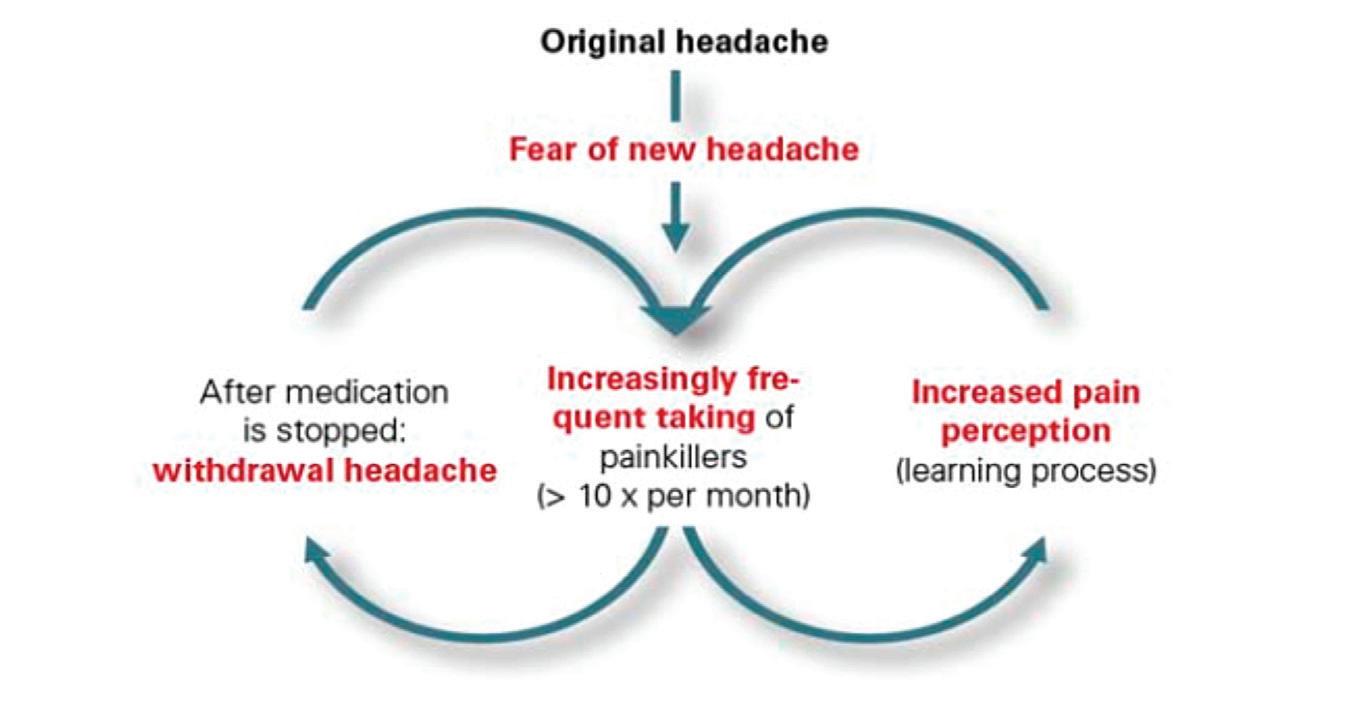
It is very important for GPs, hospital doctors (including physicians in emergency departments), associated healthcare professionals and pharmacists to consider these fundamental problems when seeing or reviewing headache patients. In 2011, a study in Ohio, US, found that excessive use of analgesic post-concussion may contribute to chronic post-traumatic headaches in some adolescents. The neuro-surgical teams in many of our hospitals in Ireland have been advised of this recently. As stated previously, many of these patients’ headaches can usually be managed more effectively once the MO issue has been addressed.
Pharmacists may be the first healthcare
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 22
FIGURE 1: The cycle of medication overuse. Image courtesy of Change Pain at www.change-pain.com
TABLE 2: Adopted from ICHD-3 diagnostic criteria for MOH *Codeine is metabolised to an opiate
MEDICATION-OVERUSE
FIRST-LINE PROPHYLACTIC THERAPIES FOR MOH IN IRELAND
1) Topiramate (25-400mg daily), beware of teratogenicity, can be used in the presence of medication overuse
2) Onabotulinum toxin A (Botox, PREEMPT protocol)#
3) CGRP treatment# – compassionate use only
4) Amitriptyline
professional to recognise patients who have MOH, as already mentioned in relation to MO, as they frequently encounter such individuals in their retail practice. Likewise, individuals with recurrent headaches who have a GMS card often come to the attention of their GP in the first instance due to the repeated requests for analgesia.
Short-term management of MO and MOH
MO and MOH (including probable MOH) have the additional potential for stigmatisation in some patients. It can put pressure on the doctor-patient relationship and blaming the patient should be avoided wherever possible. MOH should not be diagnosed in haste as it is a difficult condition to prove clinically. As outlined previously, a detailed headache and medication history should be taken meticulously, with the aim of detecting a temporal relationship between the practice of MO and the consequent worsening of the primary, usually migraine, headache disorder.
There are a number of different management strategies for dealing with MO and MOH. However, most specialists will provide the following common messages:
a) Patients need to be counselled that taking acute medication or painkillers regularly may worsen their headache problem.
b) The aim is to stop all codeine or opiate medication and reduce the number of days that triptans, NSAIDs or simple analgesia are taken (limited to four-to-six days per month, or one-to-two days each week).
c) Withdrawal or significant reduction of the offending medication is usually the first step.
d) In the short- to medium-term, this may result in an increase in headache and associated neurological symptoms and there is the additional possibility of other withdrawal symptoms.
e) Abrupt withdrawal (or significant reduction in daily use) may be possible for patients on simple analgesia.
f) A gradual reduction or weaning over weeks to months is recommended for those using codeine and/or opioid containing analgesia.
g) In our experience, many of our more chronic migraine patients with MO/MOH may benefit from psychology support. This forms part of a multidisciplinary approach and is established practice at many specialist centres internationally.
h) Having withdrawn or significantly reduced the medication that is being overused, a full assessment of the underlying headache disorder should be undertaken.
i) The patient should then be given a plan to follow for acute treatment of the primary headache condition (Table 1), which is invariably migraine.
Long-term management of MO and MOH
If the patient still has frequent and disabling migraine, they should be assessed with a view to starting prophylactic or preventive treatment. (See Table 3)
Topiramate, Botox, and the novel CGRP may work in the presence of MO, but it is desirable that MO be addressed before starting any of these treatments. Topiramate should not be used in women of childbearing age due to its teratogenic side-effects. If MOH is present, many patients will experience a long-term reduction in headache frequency after medication overuse is stopped. Access to PREEMPT Botox and CGRP treatments are generally limited. Amitriptyline does not work in the presence of MO.
Patients with MO and MOH can have complex additional medical and psychosocial needs. Typically, it takes a number of weeks (or months) for a patient to get over the withdrawal of acute medication. However, it may take much longer, especially if there is longstanding MO or there is regular opiate or codeine use. Primary care physicians may be able to identify specific patients who may need additional support or benefit from psychology (or even psychiatry) input. In some patients who have ongoing issues with MO, addictive behaviour may be involved.
While it is generally recommended that NSAID use is also limited to four-to-six days a month (or one-to-two days a week), when MOH is present, naproxen may be used in certain circumstances for a longer period. It may be helpful to give a more prolonged continuous course of naproxen 250-500mg twice daily for two-to-six weeks with appropriate cover for gastritis. More prolonged use of naproxen in this manner does not appear to be associated with MO. However, this practice should not be repeated frequently (multiple times every year) due to potential long-term side-effects of NSAIDs.
Over the years in clinical practice, patients often identify themselves that analgesia, in particular Solpadine, makes their headaches worse and they stop them themselves. Perhaps it is time for a national campaign again on MO and MOH.
Further information and support is available from the MAI, www.migraine.ie or from my website at www.marykearney.eu
References available on request
Acknowledgments:
I wish to thank Dr Martin Ruttledge, Headache Neurologist, Beaumont Hospital, Dublin; and Ms Esther Tomkins, Advanced Clinical Nurse Specialist, Beaumont Hospital, for all the work they have done on this topic, which will be presented in full in the ICGP Quick Reference Guide on Non-migraine headache disorders: Diagnosis and management from a GP perspective This guide is due to be launched shortly.
23 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
TABLE 3: Adopted from ICHD-3 diagnostic criteria for MOH #only available in specialist headache centres
An update on mindfulness: What is the evidence?
AUTHOR: Prof Brendan Kelly, Professor of Psychiatry, Trinity College Dublin
Mindfulness is everywhere. For the past decade, it has been impossible to avoid discussions about mindfulness in the media, in books, online, at work, and even in casual conversations. This is mostly good, but it sometimes seems as if mindfulness is presented as the solution to everything. It is not. Mindfulness is a very useful tool, but it is not the answer to all of life’s problems.
In its essence, mindfulness means paying attention to the present moment, simply and directly.1 It means maintaining a careful awareness of thoughts, actions and emotions, but not judging them. It involves staying focussed on the ‘now’ as much as possible and, when the mind wanders, gently re-directing it back to the present moment: The feeling of the chair, background sounds floating past, or feelings in the body.
Mindfulness means being present. While the practice is commonly associated with relaxation, mindfulness is equally associated with alertness or, more precisely, awareness, making its attainment a balancing act.
Given the ubiquity of mindfulness today, it is tempting to see it as just another over-hyped element of ‘wellness woo’, lacking substance or meaning. This is especially true when mindfulness is presented mindlessly, or touted as the solution to everything from backache to unhappiness, poor eating habits to problems with parenting.
It is important to question mindfulness in a balanced way. It is vital that we examine its purported benefits in order
to be certain that we are using our time well and not deluding ourselves with seductive world views that deliver little benefit. Evidence about mindfulness is essential, both in our own lives and across the scientific literature.
Happily, an increasing body of research supports the usefulness of mindfulness, once it is practiced properly and with commitment. There is growing evidence from randomised controlled trials that mindfulness interventions (especially eight-week mindfulness programmes) can help with the management of chronic pain, reduce rates of depressive relapse in at-risk individuals, and improve outcomes in substance abuse. 2-4
This paper examines certain developments in the mindfulness literature in 2021, looks at some of the neuroscience associated with mindfulness, and presents some conclusions for the future of this field.
Some developments in mindfulness in 2021
At present, the best clinical evidence in the field of mindfulness relates to eight-week mindfulness programmes to reduce relapse of depression in atrisk individuals. 2,3 In 2021, a review in the American Journal of Psychotherapy comprehensively synthesised the evidence for mindfulness-based cognitive therapy (MBCT), acceptance and commitment therapy (ACT), and positive psychotherapy (PPT) for treating an episode of major depression. 5 These authors performed a random-effects meta-analysis of 15
relevant studies and found that all three therapies demonstrated efficacy in reducing symptoms of depression with a small favourable effect, when compared with controls.
This finding is broadly consistent with current understandings of the usefulness of MBCT, but these authors also noted that the overall quality of evidence is low. Despite this important caveat, however, evidence to date supports the idea that MBCT and ACT may be superior to inactive or treatment-as-usual controls. In addition, PPT might be comparable to active controls for reducing symptoms of major depression after an acute course of therapy. Hopefully, continued study will clarify these benefits further.
One of the likely directions for future research is the identification of specific aspects of depression that mindfulness-based interventions (MBIs) might target. With this in mind, there was an interesting systematic review of MBIs as psychotherapy interventions for suicidality in the International Journal of Social Psychiatry in 2021.6 This review identified 13 relevant studies, comprising six randomised controlled trials, two controlled studies, and five pre-post observational studies. Findings were mostly favourable and suggested that MBIs hold promise as interventions for suicidal behaviour. Again, large scale, high-quality trials are required to clarify this, and will hopefully follow soon.
The development of the scientific literature on mindfulness was the subject of a third, especially fascinating
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 24
review paper in 2021, in the journal Mindfulness 7 This novel article presented a bibliometric analysis of publications about mindfulness indexed in Web of Science in order to identify trends and developments in mindfulness research over 55 years. The authors identified 16,581 relevant publications between 1966 and 2021, with an exponential growth in numbers since 2006.
Almost half (47 per cent) of the publications were in psychology and 21 per cent were in psychiatry. The more recent literature, between 2016 and 2021, showed a growing interest in moderators and mechanisms, long-term meditation, neuroscience, and smartphone or online delivery of interventions. It is, perhaps, neuroscience that has commanded most attention in recent years and merits further discussion here.
The effect of mindfulness on the brain
Over the past decade, there has been an explosion of neuroscientific research that seeks to correlate mindfulness practices with physical changes in the nervous system, especially the brain. 8 While this literature is still incomplete, it is now apparent that meditation practice and mindfulness affect the brain in various ways, although the extent of this is not fully clear and many studies are still small.
One magnetic resonance imaging (MRI) study examined cortical thickness in 20 experienced mindfulness meditators and 15 controls with no experience of meditation or yoga. This study found that brain regions linked with attention, interoception (perceiving sensations from inside the body), and sensory processing were thicker in meditators compared to controls.9 These findings support the idea that cortical plasticity is associated with meditation, and that sustained mindfulness practice affects the brain physically.
Another study looked at structural MRI scans and other assessments in 17 meditators and 18 controls, and found that meditators had significantly lower pain sensitivity compared to controls.10 Lower pain sensitivity was linked with thicker cortex in affective, pain-related brain regions. There was also evidence that some changes were more prominent in participants with more years’ experience of meditation, suggesting a dose-response effect. Various other studies provide similar evidence of changes in the brains of meditators, supporting the idea that sustained mindfulness meditation affects the biological brain.11
Meta-analyses and systematic reviews of the neuroscience of mindfulness
There have been a number of systematic reviews of the neuroscience of mindfulness over the past decade. Their findings are interesting and optimistic, but they also demonstrate a clear need for a broader, more coordinated literature on this topic.
One systematic review and metaanalysis of 21 neuroimaging studies in approximately 300 meditators found that eight brain regions were consistently altered in meditators, including areas related to meta-awareness (deliberate attention towards conscious thought), body awareness, memory, self and emotion regulation, and communication within the brain.13 While the ‘effect size’ was medium, the authors voiced significant concerns about selection bias, overlapping samples, and publication bias, owing to the lack of almost any negative results in the published literature. They conclude that further, more rigorous research is needed.
While studies such as these provide interesting, provocative insights into the possible effects of mindfulness and meditation on the brain, it is important to examine this literature both broadly and critically, to see if findings are consistent. The allure of brain imaging and similar research tools can lead us to mistake technology for understanding, or data for insight.12 Critical thought is vital if the pitfalls of neuroscience are to be avoided and the potential of this field is to be realised. Meta-analyses, systematic reviews and careful reflection are essential, especially when small neuroscientific studies command media attention that they might not always merit. All that glisters is not gold.
Other authors make similar points, noting positive findings, but also highlighting serious methodological problems, including small sample sizes (limiting power), variations in study design (limiting comparability), and a need for more replication of studies (confirming, refining, or refuting existing findings). 8 They conclude that future research should address these methodological difficulties and try to link the effects of mindfulness on neural structure and function with behavioural performance, such as cognitive, affective, and social function.
Fields of neuroscientific research other than neuroimaging confirm that the neuroscience of mindfulness is an area worth pursuing. One systematic review and meta-analysis examined controlled trials of the effect of mindfulnessbased interventions on brain-derived neurotrophic factor (BDNF), a biological marker of neuroplasticity.14 Despite small
25 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
They conclude that future research should address these methodological difficulties and try to link the effects of mindfulness on neural structure and function with behavioural performance
sample sizes, they found that mindfulnessbased interventions can increase peripheral BDNF, which supports the idea that mindfulness can change nervous system structure. Electroencephalography studies of electrical activity across the meditating
sustained mindfulness meditation can affect the physical brain. To date, however, studies have not characterised these effects definitively, as a result of small sample sizes, overlapping samples, selection bias, diversities of methodologies, publication
and suggesting directions for future work. It is useful to bear in mind that, notwithstanding the limitations of the scientific literature, neuroscience can neither ‘prove’ nor ‘disprove’ the value of the individual experience of mindfulness. The subjective benefits of mindfulness remain experiential, regardless of what the science finds or fails to find.
brain generally confirm this as an area of interest, albeit that methodological heterogeneity is a recurring concern.15
The future of mindfulness in medicine
Neuroscientific studies indicate that
References
bias, and failures to replicate previous studies. Hopefully, these issues will be addressed in the years to come.
During 2021, the literature on the clinical value of mindfulness expanded significantly, confirming its value
1. Kelly BD. The Doctor Who Sat For A Year. Dublin: Gill Books, 2019
2. Creswell JD. Mindfulness interventions. Annual Review of Psychology 2017; 68: 491-516
3. Segal Z, Williams M, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression (Second Edition). New York and London: The Guilford Press, 2013
4. Kelly BD. The Science of Happiness: The Six Principles of a Happy Life and the Seven Strategies for Achieving It. Dublin: Gill Books, 2021
5. Seshadri A, Orth SS, Adaji A, Singh B, Clark MM, Frye MA, McGillivray J, Fuller-Tyszkiewicz M. Mindfulness-based cognitive therapy, acceptance and commitment therapy, and positive psychotherapy for major depression. American Journal of Psychotherapy 2021; 74: 4-12
6. Raj S, Ghosh D, Verma SK, Singh T. The mindfulness trajectories of addressing suicidal behaviour: A systematic review. International Journal of Social Psychiatry 2021; 67: 507-19
7. Baminiwatta A, Solangaarachchi I. Trends and developments in mindfulness research over 55 years: A bibliometric analysis of publications indexed in Web of Science. Mindfulness 2021; 12: 2099-116
8. Tang Y-Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nature Reviews. Neuroscience 2015; 16: 213-25
9. Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway
Finally, it is important that excessive claims made about mindfulness and meditation do not draw attention away from the value of these ancient practices. As is the case with many things, mindfulness and meditation do not have all the answers, but they are useful tools when they are used with humility, awareness, and care.
Prof Kelly is the author of a number of books including The Doctor Who Sat For A Year (Gill Books)
MT, McGarvey M, Quinn BT, Dusek JA, Benson H, Rauch SL, Moore CI, Fischl B. Meditation experience is associated with increased cortical thickness. NeuroReport 2005; 16: 1893-7
10. Grant JA, Courtemanche J, Duerden EG, Duncan GH, Rainville P. Cortical thickness and pain sensitivity in Zen meditators. Emotion 2010; 10: 43-53
11. Kang D-H, Jo HJ, Jung WH, Kim SH, Jung Y-H, Choi C-H, Lee US, An SC, Jang JH, Kwon JS. The effect of meditation on brain structure: Cortical thickness mapping and diffusion tensor imaging. Social Cognitive and Affective Neuroscience 2013; 8: 27-33
12. Satel S, Lilienfeld SO. Brainwashed: The Seductive Appeal of Mindless Neuroscience. New York: Basic Books , 2013
13. Fox KCR, Nijeboer S, Dixon ML, Floman JL, Ellamil M, Rumak SP, Sedlmeier P, Christoff K. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neuroscience and Biobehavioral Reviews 2014; 43: 48-73
14. Gomutbutra P, Yingchankul N, Chattipakorn N, Chattipakorn S, Srisurapanont M. The effect of mindfulness-based intervention on brain-derived neurotrophic factor (BDNF): A systematic review and meta-analysis of controlled trials. Frontiers in Psychology 2020; 11: 2209
15. Schoenberg PLA, Vago DR. Mapping meditative states and stages with electrophysiology: Concepts, classifications, and methods. Current Opinion in Psychology 2019; 28: 211-7
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 26
Electroencephalography studies of electrical activity across the meditating brain generally confirm this as an area of interest, albeit that methodological heterogeneity is a recurring concern
Motor neurone disease in focus
AUTHOR: Theresa Lowry-Lehnen, GPN, RNP, PhD, Clinical Nurse Specialist and Associate Lecturer at Institute of Technology Carlow
Motor neurone disease (MND) is a rare, progressive, life-limiting disorder for which there is no cure, and the rate of progression varies greatly from person to person. MND refers to a group of chronic, sporadic, and hereditary neurological disorders characterised by progressive degeneration of motor neurons. Upper motor neurones, lower motor neurones, or both may be affected. Approximately 5-to-10 per cent of people diagnosed with MND have an inherited or familial form, however, the majority of people diagnosed have the sporadic form, of unknown aetiology.6,7
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, involves progressive degeneration of upper and lower motor neurones and is one of the most serious types of MND. The terms MND and ALS are often used interchangeably, however, MND is the generic term for many different types of neurological disorders, including primary lateral sclerosis (PLS), and progressive muscular atrophy (PMA), with ALS being the most prevalent.1,3 Both PLS, which affects the upper motor neurones only, and PMA, which affects the lower motor neurones only, carry a better prognosis than ALS. Individually, amyotrophy and lateral sclerosis are processes that can occur as part of several other neurological conditions, however, there are virtually no other neurological conditions except ALS in which both processes occur simultaneously. Almost 90 per cent of patients with MND have the mixed ALS form of the disease, so the terms MND and ALS have become synonymous.4
ALS is characterised by the degeneration of both upper and lower motor neurones, leading to the ultimate failure of all voluntary muscles, with rapid disease progression and a median survival rate of three years.1 Half (50 per cent) of affected patients live at least three or more years after diagnosis, 20 per cent live five years or more, and up to 10 per cent survive more than 10 years.15 Initial signs of ALS include weakness in the muscles that control swallowing, chewing, and speech. Over time, there is a weakening of
the muscles used to move the arms and legs and to hold the body upright. This muscular weakness occurs on both sides of the body. Eventually, the muscles that control breathing become so weak that those affected lose the ability to breathe on their own.3
Until recently, ALS was classified primarily within the neuromuscular domain, however, new imaging and neuropathological data have indicated the involvement of the nonmotor neuraxis in disease pathology. ALS is more accurately characterised as a group of neurodegenerative disorders that affect both the corticospinal tract and the anterior horn cell resulting in muscle denervation and atrophy. While some forms of ALS/MND are primarily motor system degenerations, evidence from genetic, clinical, and imaging studies have shown extensive overlap between ALS/MND and frontotemporal dementia (FTD).1,2 Over 50 per cent of ALS patients develop cognitive and behavioural impairment with 13-to-15 per cent presenting with co-morbid behavioural variant FTD.1,7
The Irish MND register includes all known
patients diagnosed with MND each year. The purpose of the Register is to track the incidence, prevalence and clinical features of MND in the Irish population. There are approximately 400 people living with MND in Ireland at any one time.13 The frequency of MND is relatively consistent within populations of European extraction. Around one-in-30,000 develop MND each year. In Ireland, this amounts to approximately 150 new diagnosis every year.6
The condition can affect adults of all ages, including teenagers, although this is extremely rare. It is usually diagnosed in people over 40 years of age with peak age of onset in the early 60s and it affects slightly more men than women.
Symptom onset
The symptoms of MND begin gradually over weeks and months, usually on one side of the body initially and the condition gets progressively worse. As the nerves become damaged, the muscles they control weaken and atrophy. The muscles first affected tend to be those in the hands, feet, mouth, and throat, depending on which type of the disease it is.
ALS/MND CLASSIFICATION16
CLASSICAL ALS – a progressive neurological disease characterised by a deterioration of upper and lower motor neurones. This type of ALS affects more than two-thirds of those with the disease.
PRIMARY LATERAL SCLEROSIS (PLS) – a progressive neurological disease in which the upper motor neurones deteriorate. If the lower motor neurones are not affected within two years, the disease usually remains a pure upper motor neuron disease. This is the rarest form of ALS.
PROGRESSIVE BULBAR PALSY (PBP) – a condition that starts with
difficulties in speaking, chewing and swallowing due to lower motor neurone deterioration. This disorder affects about 25 per cent of those with ALS.
PROGRESSIVE MUSCULAR ATROPHY (PMA) – a progressive neurological disease in which the lower motor neurones deteriorate. If the upper motor neurones are unaffected within two years, the disease usually remains a pure lower motor neurone disease.
FAMILIAL – a progressive neurological disease that affects more than one member of the same family. This type of ALS accounts for a very small number of people with ALS (5-to-10 per cent).
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 27
Common early symptoms include a weakened grip, which can cause difficulty picking up or holding objects; weakness at the shoulder that makes lifting the arm difficult; a ‘foot drop’ caused by weak ankle muscles; dragging of the leg and slurred speech (dysarthria). As damage progresses, symptoms spread to other parts of the body and the condition becomes more debilitating. Eventually, a person with MND may be unable to move. Communicating, swallowing, and breathing may also become very difficult. MND does not cause sensory, visual or hearing disorders, so sight, smell, touch, and hearing remain intact, as do the sphincter muscles that control the bladder and bowel. Life expectancy is variable, usually from three-to-five years after onset, depending on the activity of the disease and the particular muscle groups affected.6,7 However, some people may live for up to 10 years and in rare circumstances even longer.7
MND is often classified based on where symptom first occur. If the nerves supplying muscles in the arms, legs or trunk are affected first, it is described as ‘spinal onset’. If the nerves supplying muscles of speech or swallow are affected first, it is described as ‘bulbar onset’. Spinal onset is more common in men, and bulbar onset is more common in older women. Approximately 5 per cent of people with MND begin with difficulties catching their breath and with lying flat. This usually points to involvement of the diaphragm, and is termed ‘respiratory onset’.6
Diagnosis
There is no definitive diagnostic test for MND. Investigations are aimed at confirming the presence of upper and lower motor neurone degeneration, while excluding other conditions that could mimic the clinical presentation.1 Other conditions, such as benign cramp fasciculation syndrome, cervical radiculomyelopathy, dual pathologies, inclusion body myositis, and multifocal motor neuropathy with conduction block, can mimic MND and it is important to consider these.8 Neuroimaging is performed to exclude structural pathology and neurophysiological studies are performed to confirm the presence of acute and chronic denervation, the absence of
sensory findings and ensure mimic syndromes are excluded.1
The lack of a definitive test can cause problems, particularly if patients are seen very early after onset of symptoms, when the signs may be limited.8 In addition to a complete medical history and physical examination, diagnostic procedures for MND may include laboratory tests – including blood and urine studies and thyroid function tests; muscle and/ or nerve biopsy; cerebral spinal fluid analysis; x-rays; MRI; and electro-diagnostic tests that evaluate and diagnose disorders of the muscles and motor neurons.
Treatment and management
There is currently no cure for MND. Treatment is aimed at keeping the person comfortable, improving their quality-of-life and compensating for the progressive loss of bodily functions, such as mobility, communication, swallowing, and breathing.7 Riluzole is currently the only licenced agent that can be used to treat some forms of MND. While not a cure, research has shown that it can modestly prolong survival. It is thought to slow down the progressive damage to motor neurone cells by reducing their sensitivity to the nerve transmitter glutamate. The prescription of riluzole should only be started by a specialist who has experience in the management of MND. The standard dose of riluzole in the management of ALS is 50mg twice daily. The most common adverse effects include nausea, asthenia, and derangement in liver enzymes. Pancreatitis and fulminant hepatic failure have also been reported as rare adverse effects. Regular blood testing every month for the first three months, followed by three monthly for nine months and then yearly, is recommended. Although research has shown that sustained use of riluzole for 18 months is not associated with improved muscle strength, it has been shown to improve survival by three months, which is equitable to a 9 per cent increase in one-year survival.10
Teams of specialists use devices and therapies to help patients manage their ALS symptoms, maintain their independence and optimise their quality-of-life. Occupational and physical therapy enhances independence and helps patients with their range of motion and everyday tasks.
The nutritional care of patients is a crucial element of disease management. During the early stages of ALS, monitoring of nutritional status, assessment of swallowing, dietary advice, food fortification and provision of oral nutrition supports are all key aspects of nutritional management. With disease progression, gastrostomy feeding becomes necessary for many patients to help maintain their nutritional status.7
Speech and language therapy can help with communication and swallowing and as the ability to speak deteriorates there are technological resources and apps available to help affected individuals communicate with others. Intermittent positive pressure ventilation (IPPV) or bi-level positive airway pressure (BIPAP) can be used to aid breathing.16
Emotional lability and depression are two distinct conditions affecting some people with MND. Communication and support provided for MND patients and their caregivers, needs to pay attention to concepts of hope, control, and compassion, and how individuals may use these concepts differently to cope with the emotional impact of the disease.17
Research
Existing research points towards an underlying genetic basis in the development of ALS. Four genes are associated with up to 70 per cent of cases of familial ALS, namely the C9orf72, TARDBP, SOD1, and FUS genes. Over 25 genes and loci have been identified in relation to the predisposition of the disease, amongst which C9orf72 has been associated with 40 per cent of cases of familial and 10 per cent of cases of sporadic MND.11 Up to 10 per cent of all people diagnosed in Ireland with MND carry the abnormal C9orf72 gene, which can cause both MND and dementia.9
Stem cell therapy is a novel area of research that has fuelled hope of a treatment for a variety of conditions including MND, however, there are many unanswered questions surrounding its use. Although the use of stem cell therapy for MND may eventually be possible, the research is not sufficiently well advanced, and in Ireland embryonic stem cell research is currently not allowed.In February 2021, the University
28 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
of Edinburgh issued a press release stating that a cohort of their scientists had unveiled interesting lab results that could lead to potential future treatments. The study looked at how improving the function of mitochondria could be a possible treatment for MND. The scientists discovered that in human stem cell models of MND, the axon is shorter than in healthy cells and that the movement of the mitochondria, which travel up and down the axons, is impaired. The research showed that this was caused by a defective energy supply from the mitochondria and that by boosting the mitochondria, the axon reverted back to normal. The results of the study are now being used to look for existing drugs that boost mitochondrial function that may be able to be repurposed to treat MND.14
Several promising clinical trials are being conducted worldwide, yielding important information on how to combat MND. While the search for an effective treatment and cure continues, multidisciplinary teams across the globe assist patients and their families to adjust to the many challenges of living with ALS.
Future hopes
Last year, Prof Orla Hardiman, Professor of
References
1. Hardiman O. Management of motor neuron disease. Hospital Professional News; Issue 88; pp 48-49; September 2021
2. Hardiman O, Al-Chalabi A, Chio A, Corr E, Logroscino G, Robberecht W, Shaw P, Simmons Z, van den Berg L. Amyotrophic lateral sclerosis. 2017 Oct 5; Nat Rev Dis Primers. doi: 10.1038/ nrdp.2017.71
3. Jones D. (2014). The Difference between Motor Neuron Disease (MND) & ALS. Available at: www.griswoldhomecare.com/blog/2014/may/thedifference-between-motor-neuron-disease-mnd-/
4. OUH. (2021). What is the difference between MND and ALS? Oxford University Hospital, UK. Available at: www.ouh.nhs.uk/services/departments/ neurosciences/neurology/mnd/support/mnd-als.aspx
5. HIQA. (nd). Irish Motor Neurone Disease Register. Available at: www.hiqa.ie/areas-we-work/ health-information/data-collections/irish-motorneurone-disease-register
6. IMNDA. (2019). Facts about MND. Irish Motor Neurone Disease Association. Available at: https://
Neurology and Head of the Academic Unit of Neurology at Trinity College and Consultant Neurologist at Beaumont Hospital, Dublin, noted that Ireland, along with other countries in Europe, have committed to a number of exciting new MND clinical trials. “These include trials performed in collaboration with pharmaceutical companies, and trials of drugs that have been selected by our European Clinical Trials Consortium. The drugs that have been selected work on many different pathways in MND. The sheer number of new drugs ready for clinical trial allow us to be confident that we will make real breakthroughs to treat MND in the near future.”14
Referring to future technologies and advancements in the treatment of MND Prof Hardiman states: “It is axiomatic that future treatments will require a precision medicine based approach, but overcoming the factors that have limited the success of translational medicine will also require novel solutions. ALS/MND is a rare disease, and we now know that it comprises many different subtypes with different pathobiologic mechanisms. The next step in Ireland is to lead on the development of a system that enables collection and uploading of human data at a very large
imnda.ie/about-mnd/more-facts-aboutmotor-neurone-disease/
7. NHS Inform (2021). Motor neurone disease (MND). NHS Inform, Scotland. Available at: www. nhsinform.scot/illnesses-and-conditions/brainnerves-and-spinal-cord/motor-neurone-disease-mnd
8. McDermott C, Shaw P. Diagnosis and management of motor neurone disease. BMJ 2008 Mar 22; 336(7645): 658 662. doi: 10.1136/ bmj.39493.511759.BE
9. Trinity researchers in breakthrough trial for motor neuron disease. Trinity News and Events, September 2020. Available online at: www.tcd. ie/news_events/articles/trinity-researchers-inbreakthrough-trial-for-motor-neuron-disease/
10. Dharmadasa T, Kiernan M. Riluzole, disease stage and survival in ALS. The Lancet Neurology 2018 May; [PubMed PMID: 29525493]
11. Renton A, Chiò A,Traynor B. State of play in amyotrophic lateral sclerosis genetics. Nature Neuroscience. 2014 Jan; [PubMed PMID: 24369373]
12. Arora R. (2021). Motor neuron disease. Continuing education activity. Available
scale across Europe, delivering a wealth of new multimodal, multisource, clinical phenotype and outcome, imaging, neuro electric signalling, biochemical and genomic datasets that will ultimately help to inform how we categorise each patient. This in turn will inform how we design and test new treatments using an exciting array of new and emerging technologies.”1 ■
Cork University Press in collaboration with the Irish Motor Neurone Disease Association has recently published Living with Motor Neurone Disease: A Complete Guide edited by Dr Marie Murray, and written by many of the most distinguished Irish experts on MND, bringing safe, reliable, practical information and reassurance to everyone affected by MND.
This is a step-by-step guide for everyone, including healthcare staff, patients and family/caregivers. In summary, it is an invaluable resource to inform, educate prepare and signpost people toward practical everyday supports and clinical expertise.
at: www.statpearls.com/ArticleLibrary/ viewarticle/25287#ref_24369373
13. IMNDA (2019). Commonly asked questions. Irish Motor Neurone Disease Association. Available at: https://imnda.ie/ just-diagnosed/faqs/
14. IMNDA (2021). NEW YEAR – NEW RESEARCH UPDATES! Irish Motor Neurone Disease Association. Available at: https://imnda.ie/new-year-newresearch-updates/
15. Medscape (2018). Amyotrophic lateral sclerosis. Available at: https://emedicine.medscape.com/ article/1170097-overview
16. John Hopkins Medicine (nd). ALS –amyotrophic lateral sclerosis. Available at: www.hopkinsmedicine.org/neurology_neurosurgery/ centers_clinics/als/conditions/als_amyotrophic_ lateral_sclerosis.html
17. Pinto C, Geraghty A, Yardley L, et al. Emotional distress and well-being among people with motor neurone disease (MND) and their family caregivers: A qualitative interview study. BMJ Open 2021;11: e044724. doi: 10.1136/bmjopen-2020-044724
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 29
Neurophobia and its implications for the Irish healthcare system
AUTHORS: John Inocentes, Clinical Research Nurse, Dublin Neurological Institute; and Prof Timothy Lynch, Consultant Neurologist, Mater Misericordiae University Hospital and Clinical Director of the Dublin Neurological Institute
Neurophobia is a phenomena defined as the fear of neurology among different medical professionals ranging from medical students, speech and language therapists, occupational therapists, to primary care physicians (Flanagan et al, 2007, Keane et al, 2018).
Over the last two decades, research has sought to identify neurophobia and the implications it bears on the broader healthcare system. While seemingly harmless, the tainted perceptions of neurology as an overly complex and difficult branch of medicine affects different cohorts of healthcare professionals and their practice. In medical students, neurophobia manifests as an inability to utilise basic neurological knowledge while providing bedside care. This fear of neurology further develops in the careers of the medical student and contributes to the steady decline of doctors entering the field of neuroscience (Shelley et al, 2018). There is a lack of neurologists all throughout the globe from Canada, US, New Zealand, the UK, and to other European countries (Burton, 2018). In Ireland, this shortage is highlighted by the alarming ratios of neurologists per head of population. The UK recommended ratio is one neurologist per 70,000 population. However, in Ireland this ratio is almost twice as much at one neurologist per 130,000 population on average per region. (Report on the First Patient Experience Survey of Neurology Services in Ireland, 2018).
Not only does neurophobia contribute to the manpower shortages that exist globally and locally, it also affects
how primary care physicians deal with patients with neurological disorders. Studies suggest that primary care physicians and GPs are anxious and have less confidence in treating patients with neurological disorders (McCarron et al, 2014, Flanagan et al, 2007). Through a neurophobic lens, this group of physicians view patients with these disorders to be complex and difficult to diagnose and manage (Loftus et al, 2016, Flanagan et al, 2007). In practice, the lack of confidence in dealing with neurology patients leads
GPs to refer patients to a consultant neurologist to address problems that could be solved at a primary care level. While these referrals can contain simple queries regarding diagnosis, management, or treatment, they ultimately contribute to the ever-growing waiting list that an already understaffed service must filter through.
In July 2020, there were approximately 22,456 Irish patients waiting to be seen
by a neurologist. In the last five years alone, 9,238 patients have been added to the countrywide neurology outpatient waiting list, a concerning 70 per cent increase from 2015 figures. In reference to these figures, the Neurological Alliance of Ireland (NAI) acknowledges that this exponential growth is unsustainable given the existing resources available (Report on the First Patient Experience Survey of Neurology Services in Ireland, 2018). An overpopulated waiting list essentially means that patients suffer from a delay in diagnosis, management or treatment. Moreover, based on latest available data, one-in-three Europeans are set to live with or develop brain disorders in their lifetime and in Europe alone neurological disorders make up 35 per cent of Europe’s total disease burden with a yearly cost of €798 billion (Olsen et al, 2012). Given the trajectory of new neurology cases and the economic consequences of these disorders it is essential to find innovate solutions to address these problems head on. While there is no one quick solution to solve the shortage of neurologists or the ever-growing neurology waiting lists in Ireland, combating neurophobia in our medical professionals is a viable route moving forward.
Combating neurophobia
In recent studies tackling neurophobia, the focus is on changing the way medical professionals engage with concepts in neurology. It had been proposed that changes in teaching methods and the tools used to teach neurology can combat misconceptions about this particular branch in medicine (Sandrone et al, 2019, Shelley et al, 2018). As one of the
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 30
The UK recommended ratio is one neurologist per 70,000 population. However, in Ireland this ratio is almost twice as much at one neurologist per 130,000 population on average per region
few centres for neurology in Ireland, the Dublin Neurological Institute (DNI) at the Mater Misericordiae University Hospital in partnership with University College Dublin, has taken up the
services to support these medical professionals as they see neurology patients in the community. Aside from seasonal GP lectures tackling different concepts in neurology, the DNI at the
practice. Initially inspired by the Virtual Heart Consultation Clinics (VHCC) established by Prof Ken McDonald, Consultant Cardiologist and Medical Director of the Heartbeat Trust and Prof Jim O’Neil, Consultant Cardiologist at the Mater Misericordiae University Hospital, the DNI at the Mater has noted the success of this service and hopes to recreate the positive impacts that the VHCC provides. By supporting and educating GPs and other allied professionals we aim to change perceptions of neurology in the Irish healthcare system and eliminate neurophobia, one medical professional at a time.
challenge to combat neurophobia in our medical community through innovative approaches in education and knowledge dissemination.
As a way to address neurophobia in GPs, the DNI has created complementary
References
1. Burton A. (2018). How do we fix the shortage of neurologists? The Lancet Neurology, 6, 502-503. doi.org/10.1016/ s1474-4422(18)30143-1
2. Conway S, Tubridy N. (2018). ‘Neurophobia’: More nurture than nature? Ir Med J, 111(3):710. https://imj.ie/ neurophobia-more-nurture-than-nature/
3. Flanagan E, Walsh C, Tubridy N. (2007). Neurophobia – attitudes of medical students and doctors in Ireland to neurological teaching. Eur J Neurol, 10, 1109-1112. doi.org/10.1111/j.14681331.2007.01911.x
4. Javaid MA, Chakraborty S, Cryan JF, Schellekens H, Toulouse A. (2017a).
Understanding neurophobia: Reasons behind impaired understanding and learning of neuroanatomy in crossdisciplinary healthcare students. Anatomical Sciences Education, 1, 81-93. doi.org/10.1002/ase.1711
5. Keane C, McClelland S, Gallagher
Mater have launched a new Neurology Virtual Consultation Clinic, which allows GPs and other allied healthcare professionals direct access to expert consultant neurologists to discuss any questions they may have about any neurology patients they see in their
If you are a part of a GP practice or know of a GP practice that would like to engage with the Neurology Virtual Consultation Clinic you can contact us at DNIVirtualNeurology@mater.ie or call (01) 854 5260.
J, O’Reilly O, Fawsitt R, Ledwidge M, McDonald K. (2018). The heart failure virtual consultation – a powerful tool for the delivery of specialist care and the democratisation of knowledge in the community. Eur J Heart Fail, 2, 255-256. doi.org/10.1002/ejhf.1390
6. Loftus AM, Wade C, McCarron MO. (2016). Primary care perceptions of neurology and neurology services. Postgraduate Medical Journal, 1088, 318–321. doi.org/10.1136/ postgradmedj-2015-133683
7. McCarron MO, Stevenson M, Loftus AM, McKeown P. (2014). Neurophobia among general practice trainees: The evidence, perceived causes and solutions. Clin Neurol Neurosurg, 124-128. doi.org/10.1016/j. clineuro.2014.03.021
8. Olesen J, Gustavsson A, Svensson M, Wittchen HU, Jönsson B; CDBE2010 study group, and European Brain Council (2012). The economic cost of brain disorders in Europe. Eur J Neurol, 19(1), 155-162. doi.
org/10.1111/j.1468-1331.2011.03590.x
9. Social Justice Ireland. (2020, August 31). Outpatient waiting lists exceed 600,000 in July 2020 while Covid-19 cases rise. www.socialjustice.ie/content/policyissues/outpatient-waiting-lists-exceed600000-july-2020-while-covid-19-cases-rise
10. Neurological Alliance of Ireland. (2018). Report on the first patient experience survey of neurology services in Ireland. www.Nai.Ie/Assets/58/303585F0-3BCE-4C938FBA6C71174F62A5_document/Final_report.Pdf
11. Sandrone S, Berthaud JV, Chuquilin M, Cios J, Ghosh P, Gottlieb-Smith RJ, et al. (2018). Neurologic and neuroscience education. Neurology, 4, 174-179. doi. org/10.1212/wnl.0000000000006716
12. Shelley BP, Chacko TV, Nair BR. (2018). Preventing ‘neurophobia’: Remodeling neurology education for 21st Century medical students through effective pedagogical strategies for ‘neurophilia’. Ann Indian Acad Neurol, 21(1), 9-18. doi.org/10.4103/aian.AIAN_371_17
31 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
As a way to address neurophobia in GPs, the DNI has created complementary services to support these medical professionals as they see neurology patients in the community
A STEP FORWARD
A STEP FORWARD
INTRODUCING ONGENTYS® (OPICAPONE) TO IRELAND
INTRODUCING ONGENTYS® (OPICAPONE) TO IRELAND



Thursday 3rd February 2022, 18:30-20:00
Thursday 3rd February 2022, 18:30-20:00
Register now for our live webinar to learn more about the use of ONgentys® in your PD Practice
To register please go to: bit.ly/ASTEPFORWARD or scan the QR code: agenda
18:30
18:30 WELCOME AND INTRODUCTIONS
To register please go to: bit.ly/ASTEPFORWARD or scan the QR code: agenda
WELCOME AND INTRODUCTIONS
Professor Tim Lynch, Dublin Neurological Institute at the Mater Misericordiae University Hospital
Professor Tim Lynch, Dublin Neurological Institute at the Mater Misericordiae University Hospital
18:40 THE USE OF COMT INHIBITORS IN PARKINSON’S Professor Peter Jenner, King’s College London
18:40 THE USE OF COMT INHIBITORS IN PARKINSON’S Professor Peter Jenner, King’s College London


19:15 ONGENTYS PIVOTAL STUDIES AND LATEST TRIALS
19:15 ONGENTYS PIVOTAL STUDIES AND LATEST TRIALS
Professor Joaquim Ferreira, University of Lisbon
Professor Joaquim Ferreira, University of Lisbon




19:50 Q&A PANEL 20:00 CLOSE
19:50 Q&A PANEL 20:00 CLOSE
Register now for our live webinar to learn more about the use of ONgentys® in your PD Practice This webinar is for healthcare professionals only and is organised and funded by
Prescribing information can be found on the following page
Prescribing information can be found on the following page
UK/ON/2021/057g
UK/ON/2021/057g
Date of preparation: January 2022
Date of preparation: January 2022
This webinar is for healthcare professionals only and is organised and funded by
Prescribing information
Ongentys® (opicapone)
Ongentys® (opicapone)
Please refer to the SPC before prescribing. Presentation: Capsules containing 50 mg of opicapone. Indication: Adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors (DDCI) in adult patients with Parkinson’s disease and end-of-dose motor fluctuations who cannot be stabilised on those combinations. Dosage and administration: The recommended dose is 50 mg of opicapone. It should be taken once daily at bedtime at least one hour before or after levodopa combinations. Ongentys is to be administered as an adjunct to levodopa treatment and enhances the effects of levodopa. Hence, it is often necessary to adjust levodopa dosage by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating the treatment with opicapone according to the clinical condition of the patient. If one dose is missed, the next dose should be taken as scheduled. The patient should not take an extra dose to make up for the missed dose. Elderly patients: No dose adjustment is needed for elderly patients. Caution must be exercised in patients ≥ 85 years of age as there is limited experience in this age group. Patients with renal impairment: No dose adjustment is necessary in patients with renal impairment, as opicapone is not excreted by the kidney. Patients with hepatic impairment: No dose adjustment is necessary in patients with mild hepatic impairment (ChildPugh Class A). There is limited clinical experience in patients with moderate hepatic impairment (Child- Pugh Class B). Caution must be exercised in these patients and dose adjustment may be necessary. There is no clinical experience in patients with severe hepatic impairment (Child-Pugh Class C), therefore, Ongentys is not recommended in these patients. Contraindications: Hypersensitivity to the active substance or to any of the excipients. Phaeochromocytoma, paraganglioma, or other catecholamine secreting neoplasms. History of neuroleptic malignant syndrome and/or non-traumatic rhabdomyolysis. Concomitant use with monoamine oxidase (MAO-A and MAO-B) inhibitors (e.g. phenelzine, tranylcypromine and moclobemide) other than those for the treatment of Parkinson’s disease. Pregnancy: Ongentys is not recommended during pregnancy and in women of childbearing potential not using contraception. Lactation: Breast-feeding should be discontinued during treatment with Ongentys. Warnings and precautions: Opicapone enhances the effects of levodopa. To reduce levodopa-related dopaminergic adverse reactions (e.g. dyskinesia, hallucinations, nausea, vomiting and orthostatic hypotension), it is often necessary to adjust the daily dose of levodopa by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating treatment with Ongentys, according to the clinical condition of the patient. Patients and care-givers should be made aware that impulse control disorders including pathological gambling, increased libido, hypersexuality, compulsive spending or buying, binge eating and compulsive eating can occur in patients treated with dopamine agonists and/or other dopaminergic treatments. Patients should be monitored regularly for the development of impulse control disorders and review of treatment is recommended if such symptoms develop. Increases in liver enzymes were reported in studies nitrocatechol inhibitors of catechol -O -methyltransferase (COMT). For patients who experience progressive anorexia,
Please refer to the SPC before prescribing. Presentation: Capsules containing 50 mg of opicapone. Indication: Adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors (DDCI) in adult patients with Parkinson’s disease and end-of-dose motor fluctuations who cannot be stabilised on those combinations. Dosage and administration: The recommended dose is 50 mg of opicapone. It should be taken once daily at bedtime at least one hour before or after levodopa combinations. Ongentys is to be administered as an adjunct to levodopa treatment and enhances the effects of levodopa. Hence, it is often necessary to adjust levodopa dosage by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating the treatment with opicapone according to the clinical condition of the patient. If one dose is missed, the next dose should be taken as scheduled. The patient should not take an extra dose to make up for the missed dose. Elderly patients: No dose adjustment is needed for elderly patients. Caution must be exercised in patients ≥ 85 years of age as there is limited experience in this age group. Patients with renal impairment: No dose adjustment is necessary in patients with renal impairment, as opicapone is not excreted by the kidney. Patients with hepatic impairment: No dose adjustment is necessary in patients with mild hepatic impairment (ChildPugh Class A). There is limited clinical experience in patients with moderate hepatic impairment (Child- Pugh Class B). Caution must be exercised in these patients and dose adjustment may be necessary. There is no clinical experience in patients with severe hepatic impairment (Child-Pugh Class C), therefore, Ongentys is not recommended in these patients. Contraindications: Hypersensitivity to the active substance or to any of the excipients. Phaeochromocytoma, paraganglioma, or other catecholamine secreting neoplasms. History of neuroleptic malignant syndrome and/or non-traumatic rhabdomyolysis. Concomitant use with monoamine oxidase (MAO-A and MAO-B) inhibitors (e.g. phenelzine, tranylcypromine and moclobemide) other than those for the treatment of Parkinson’s disease. Pregnancy: Ongentys is not recommended during pregnancy and in women of childbearing potential not using contraception. Lactation: Breast-feeding should be discontinued during treatment with Ongentys. Warnings and precautions: Opicapone enhances the effects of levodopa. To reduce levodopa-related dopaminergic adverse reactions (e.g. dyskinesia, hallucinations, nausea, vomiting and orthostatic hypotension), it is often necessary to adjust the daily dose of levodopa by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating treatment with Ongentys, according to the clinical condition of the patient. Patients and care-givers should be made aware that impulse control disorders including pathological gambling, increased libido, hypersexuality, compulsive spending or buying, binge eating and compulsive eating can occur in patients treated with dopamine agonists and/or other dopaminergic treatments. Patients should be monitored regularly for the development of impulse control disorders and review of treatment is recommended if such symptoms develop. Increases in liver enzymes were reported in studies nitrocatechol inhibitors of catechol -O -methyltransferase (COMT). For patients who experience progressive anorexia,
UK/ON/2021/057g
asthenia and weight decrease within a relatively short period of time, a general medical evaluation including liver function should be considered. Excipients: Ongentys contains lactose. Patients with rare hereditary problems of galactose intolerance, the total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product. Drug interactions: Concomitant use of opicapone with MAO inhibitors (e.g. phenelzine, tranylcypromine and moclobemide) other than those for the treatment of Parkinson’s disease is contraindicated. Concomitant use of opicapone and MAO inhibitors for the treatment of Parkinson’s disease, e.g. rasagiline (up to 1 mg/day) and selegiline (up to 10 mg/day in oral formulation or 1.25 mg/day in buccal absorption formulation), is permissible. There is no experience with opicapone when used concomitantly with the MAO-B inhibitor safinamide. Therefore, their concomitant use should be considered with appropriate caution. Opicapone may interfere with the metabolism of medicinal products containing a catechol group that are metabolised by COMT, e.g. rimiterole, isoprenaline, adrenaline, noradrenaline, dopamine, dopexamine or dobutamine, leading to potentiated effects of these medicinal products. Careful monitoring of patients being treated with these medicinal products is advised when opicapone is used. Concomitant use with tricyclic antidepressants and noradrenaline re-uptake inhibitors (e.g. venlafaxine, maprotiline and desipramine) should be considered with appropriate caution. Particular consideration should be given to medicinal products metabolised by CYP2C8 and their co-administration must be avoided. Particular consideration should be given to medicinal products transported by OATP1B1 and their concomitant use should be considered with appropriate caution Adverse events: Refer to the SPC for all side effects. Very common side effects (≥ 1/10): Dyskinesia. Common side effects (≥ 1/100 to < 1/10): Abnormal dreams, Hallucination, Hallucination visual, Insomnia, Dizziness, Headache, Somnolence, Orthostatic hypotension, Constipation, Dry mouth, Vomiting, Muscle spasms, Blood creatine phosphokinase increased. Uncommon side effects (≥ 1/1,000 to < 1/100): Decreased appetite, Hypertriglyceridaemia, Anxiety, Depression, Hallucination auditory, Nightmares, Sleep disorder, Dysgeusia, Hyperkinesia, Syncope, Dry eye, Ear congestion, Palpitations, Hypertension, Hypotension, Dyspnoea, Abdominal distention, Abdominal pain, Abdominal pain upper, Dyspepsia, Muscle twitching, Musculoskeletal stiffness, Myalgia, Pain in extremity, Chromaturia, Nocturia, Weight decreased. Legal Category: POM. Basic UK NHS cost: Ongentys pack of 30: £93.90. Marketing authorisation numbers: PLGB 21566/0004 EU/1/15/1066/003. Marketing authorisation holder: Bial-Portela & Ca., S.A., A Avenida da Siderurgia nacional 4745-457 Coronado (S. Romao e S. Mamede) – Portugal. Further Information from: Bial Pharma UK Ltd., Admiral House, St. Leonard’s Road, Windsor, SL4 3BL, UK. Job code: UK/ON/2021/016(1). Date of preparation: October 2021.
asthenia and weight decrease within a relatively short period of time, a general medical evaluation including liver function should be considered. Excipients: Ongentys contains lactose. Patients with rare hereditary problems of galactose intolerance, the total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product. Drug interactions: Concomitant use of opicapone with MAO inhibitors (e.g. phenelzine, tranylcypromine and moclobemide) other than those for the treatment of Parkinson’s disease is contraindicated. Concomitant use of opicapone and MAO inhibitors for the treatment of Parkinson’s disease, e.g. rasagiline (up to 1 mg/day) and selegiline (up to 10 mg/day in oral formulation or 1.25 mg/day in buccal absorption formulation), is permissible. There is no experience with opicapone when used concomitantly with the MAO-B inhibitor safinamide. Therefore, their concomitant use should be considered with appropriate caution. Opicapone may interfere with the metabolism of medicinal products containing a catechol group that are metabolised by COMT, e.g. rimiterole, isoprenaline, adrenaline, noradrenaline, dopamine, dopexamine or dobutamine, leading to potentiated effects of these medicinal products. Careful monitoring of patients being treated with these medicinal products is advised when opicapone is used. Concomitant use with tricyclic antidepressants and noradrenaline re-uptake inhibitors (e.g. venlafaxine, maprotiline and desipramine) should be considered with appropriate caution. Particular consideration should be given to medicinal products metabolised by CYP2C8 and their co-administration must be avoided. Particular consideration should be given to medicinal products transported by OATP1B1 and their concomitant use should be considered with appropriate caution Adverse events: Refer to the SPC for all side effects. Very common side effects (≥ 1/10): Dyskinesia. Common side effects (≥ 1/100 to < 1/10): Abnormal dreams, Hallucination, Hallucination visual, Insomnia, Dizziness, Headache, Somnolence, Orthostatic hypotension, Constipation, Dry mouth, Vomiting, Muscle spasms, Blood creatine phosphokinase increased. Uncommon side effects (≥ 1/1,000 to < 1/100): Decreased appetite, Hypertriglyceridaemia, Anxiety, Depression, Hallucination auditory, Nightmares, Sleep disorder, Dysgeusia, Hyperkinesia, Syncope, Dry eye, Ear congestion, Palpitations, Hypertension, Hypotension, Dyspnoea, Abdominal distention, Abdominal pain, Abdominal pain upper, Dyspepsia, Muscle twitching, Musculoskeletal stiffness, Myalgia, Pain in extremity, Chromaturia, Nocturia, Weight decreased. Legal Category: POM. Basic UK NHS cost: Ongentys pack of 30: £93.90. Marketing authorisation numbers: PLGB 21566/0004 EU/1/15/1066/003. Marketing authorisation holder: Bial-Portela & Ca., S.A., A Avenida da Siderurgia nacional 4745-457 Coronado (S. Romao e S. Mamede) – Portugal. Further Information from: Bial Pharma UK Ltd., Admiral House, St. Leonard’s Road, Windsor, SL4 3BL, UK. Job code: UK/ON/2021/016(1). Date of preparation: October 2021.
Adverse events should be reported.
Reporting forms and information can be found at www.yellowcard.mhra.gov.uk or in Ireland: www.hpra.ie.
Adverse events should also be reported to BIAL on +44 (0)1628 531171 or bial@pharmalex.com
Adverse events should be reported. Reporting forms and information can be found at www.yellowcard.mhra.gov.uk or in Ireland: www.hpra.ie. Adverse events should also be reported to BIAL on +44 (0)1628 531171 or bial@pharmalex.com
Date of preparation: January 2022
UK/ON/2021/057g
Date of preparation: January 2022
Prescribing information
The psychiatric impact of post-Covid-19 syndrome
AUTHORS: Prof Brendan Kelly, Professor of Psychiatry, Trinity College Dublin; and Prof Gautam Gulati, Consultant Forensic Psychiatrist, and Adjunct Professor at the University of Limerick
The Covid-19 pandemic has brought extensive changes to the lives of everyone around the world. Even people who do not contract the virus themselves find their worlds transformed: family members ill or deceased, public health restrictions limiting activities, lives and livelihoods under threat, and free-floating anxiety everywhere. It is an extraordinary time, not least because of the prominence that personal and public health have taken in our day-to-day lives. Issues relating to personal and social responsibility dominate the airwaves, and everyone has learned a new language, from ‘flattening the curve’ to the ‘R number’.
This article focuses on certain aspects of the impact of the pandemic on mental health and, especially, the longer-term psychiatric consequences of infection with Covid-19. In particular, it explores the concept of ‘postCovid-19 syndrome’, which is increasingly recognised as one of the potential sequelae of acute Covid-19.
Covid-19 and mental health
Unsurprisingly, the Covid-19 pandemic has had a substantial impact on mental health. Evidence to date indicates that the combined effects of the pandemic itself and the public health restrictions it necessitates have resulted in approximately one person in every five in the general population experiencing significantly increased psychological distress. This distress commonly manifests as anxiety, stress, and symptoms of depression.
The rate of this distress is remarkably consistent across countries, cultures and various different settings. In some ways, we are more similar than we think, especially when confronted with a common challenge, such as the pandemic. Even so, particular risk factors for poor mental health during Covid-19 have been identified, including being female and living alone. This is an especially difficult time
for people who had limited social connections prior the pandemic. The advent of Covid-19 has had a particular impact on them as a result of quarantine orders, social distancing, and general limits on services and interactions. They require additional support.
Among healthcare workers, rates of psychological distress during the pandemic are approximately double those in the general population. Much of this distress is understandable in the context of the medical emergency triggered by the virus. This has led to longer working hours for many healthcare workers, changing shift patterns, increased pressures in the workplace, and ongoing concerns about infection. These are in addition to further pandemic-related complexities in the personal lives of healthcare and other workers as a result of restrictions, school closures, family members falling ill, and all of the other consequences of the public health emergency.
Regrettably, many of the steps required to alleviate these problems among healthcare workers are more difficult in a pandemic: careful rostering, ability to take leave, organisational support from employers, and ‘psychological first aid’ for those in distress. Despite the challenges, all of these measures can help to ameliorate the pressures faced by healthcare workers and other frontline staff, once they are supported by specialist mental healthcare for people who are in particular need. Collegial support is especially important during these difficult times.
In addition to the general stresses of the pandemic, and those specific to healthcare workers, Covid-19 infection itself impacts on mental health in both the short-term (eg, anxiety, depression) and the longer-term, especially among those who are hospitalised. These longer-term consequences can include persistent anxiety, post-traumatic stress,
post-viral syndromes and various other manifestations of poor mental health.
People with pre-existing mental illness are at particular risk of infection with Covid-19 and require additional support both during the pandemic and in its aftermath. Often people with chronic mental illness experience difficulty accessing regular health services and preventive care, both of which are especially important at this time.
Mental health and post-Covid-19
From the outset, it was clear that the Covid-19 pandemic was likely to affect mental health significantly. What is increasingly apparent, however, is that ‘post-Covid-19 syndrome’ is more common and more potentially disabling than many might have expected. In addition, it is also now clear that this syndrome has significant psychological and psychiatric dimensions that merit close attention and careful management. While information is still relatively scarce, it is useful to reflect on what we know at this point. More information will surely follow.
Within the first year of the pandemic, many clinicians observed that some Covid-19 patients had persistent symptoms of the infection, even after the acute illness had improved and the patient had apparently recovered. Common persisting symptoms included fatigue, shortness of breath, joint pain, chest pain, and diminished quality-of-life. It is now clear that, for many patients, these lingering effects of the virus are substantial, disabling, and persistent.
In light of a growing body of evidence along these lines, the UK’s National Institute for Health and Care Excellence (NICE) published an up-to-date Covid-19 rapid guideline: Managing the long-term effects of Covid-19 in November 2021, in collaboration with the Scottish Intercollegiate Guidelines Network
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 34
(SIGN) and the Royal College of General Practitioners (RCGP). This guidance provides as much clarity as is possible at the moment, given the evolving state of evidence in this field. Experience with the longer-term effects of Covid-19 is necessarily limited, but knowledge is growing every month.
One of the most useful parts of the guidance from NICE, SIGN and RCGP is its clarification of the terminology used to describe the persistent effects of Covid-19. The document states that post-Covid-19 syndrome is present when signs and symptoms that develop during or after an infection consistent with Covid-19 last for more than 12 weeks and are not better explained by an alternative diagnosis. Often, there are clusters of symptoms, which commonly overlap, can fluctuate, can change over time, and can impact on any body system.
The term ‘long Covid’ describes signs and symptoms that continue or develop after acute Covid-19 infection, and this term therefore includes both ongoing symptomatic Covid-19 (from four-to-12 weeks) and post- Covid-19 syndrome (12 weeks or more).
The epidemiology of post-Covid-19
At this point, as 2022 begins, more than 250 million people around the world have been infected by Covid-19. Over five million have died. These statistics are likely to be underestimates, owing to difficulties with diagnosis in many places, suboptimal health services in certain parts of the world, and uneven reporting systems. Future studies are likely to determine that the incidence was higher.
Even based on the figures we have today, however, it is clear that some hundreds of millions of people will be at risk of postCovid-19 syndrome after this pandemic ends. The implications for public health are enormous. The prominence of psychological and psychiatric symptoms in this syndrome suggests that the implications for public mental health will form an especially challenging part of the work that lies ahead.
With this in mind, it is important to establish
precisely how common post-Covid-19 syndrome is, in order to estimate future healthcare need. One cohort study followed up 277 Covid-19 patients and identified post-acute Covid-19 syndrome in 50.9 per cent of them between 10 and 14 weeks after disease onset. Radiological and spirometric changes tended to be mild and were found in less than 25 per cent of patients. By way of contrast, over one-third of these patients experienced fatigue and two-thirds of those with post-acute Covid-19 syndrome reported diminished quality-of-life. Clearly, this is a syndrome with substantial psychological and neuro-psychiatric components that are significantly disabling for many sufferers.
Symptoms of poor mental health are present even in the early stages after acute infection. Studies conducted two weeks after physical recovery from Covid-19 detect high levels of anxiety (22 per cent), depression (21 per cent) and post-traumatic stress disorder (20 per cent) among patients. Over one-third (36 per cent) report psychological distress and a similar proportion (35 per cent) have sleep disorders. These problems appear to be more common among survivors of Covid-19 than certain other infections. Rates of anxiety and depression following Ebola, for example, are 14 per cent and 15 per cent, respectively, compared to 22 per cent and 21 per cent with Covid-19. It is not entirely clear why Covid-19 is especially corrosive of mental health, but it is.
To compound matters, these psychiatric sequelae of Covid-19 tend to persist. In the first six months after infection, one-third of patients have a neurological or psychiatric diagnosis, increasing to almost half (46.4 per cent) of those admitted to intensive therapy units. Anxiety disorders, in particular, are present in 17.4 per cent of all Covid-19 patients during this period, and 19.1 per cent of those admitted to intensive therapy units. Again, these problems appear more common following Covid-19 than other infections. For example, the risk of psychosis following Covid-19 is twice as high as it is following influenza. Again, Covid-19 presents a particular risk to mental health, even in its aftermath.
Most healthcare professionals are familiar with different post-viral syndromes that affect our patients to varying degrees. The mental health consequences of Covid-19, however, appear especially common and severe, and therefore the challenges to mental health services and public mental health will be even greater. Even the bare numbers of people affected by Covid-19 are sufficient to confirm that post-Covid-19 syndrome will be a health issue of the greatest magnitude in the years ahead.
So, what can we do now?
In the first instance, adhering to public health guidance, promoting vaccination, and supporting good general health are all important preventive measures for Covid-19 in the first place. Prompt diagnosis and treatment of Covid-19 infection is also vital. The basics still matter and will hopefully prevent yet more people being at risk of post-Covid-19 syndrome in the future.
Second, we need to identify post-Covid psychiatric symptoms as early as feasible and provide appropriate multidisciplinary care. There is very little evidence about the usefulness of specific psychiatric treatments during the post-Covid period in particular, but the usual principles of bio-psycho-social psychiatry will clearly still apply.
Third, we need more data. Longitudinal studies are essential to better understand post-Covid-19 syndrome, calculate its incidence, estimate the public health impact, and – hopefully – identify specific interventions that work. The need for information has never been greater. Now that this syndrome is recognised, this information can hopefully be gathered and used to relieve the considerable suffering associated with the condition.
References on request
Prof Kelly is author of The Science of Happiness: The Six Principles of a Happy Life and the Seven Strategies for Achieving It (Gill Books, 2021); Prof Gulati is co-author of Psychiatry Algorithms in Primary Care (Wiley-Blackwell, 2021)
35 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
An update from FutureNeuro SFI Research Centre
AUTHORS: Prof David Henshall, FutureNeuro Centre Director and Professor of Molecular Physiology and Neuroscience at the RCSI University of Medicine and Health Sciences; Ciara Courtney, Communications and Education and Public Engagement Lead, FutureNeuro; and Bridget Doyle, Centre and Business Development Manager, FutureNeuro
According to the Neurological Association of Ireland (NAI), there are over 800,000 people in Ireland living with a neurological condition. Brain diseases have a devastating impact on people living with neurological conditions, their families and carers. They are estimated to cost the economy €3 billion each year. The FutureNeuro SFI Research Centre was established in 2017 to address the significant unmet needs of people living with chronic and rare neurological disorders and to support the health professionals who care for them.
FutureNeuro is hosted by the RCSI University of Medicine and Health Sciences, with researchers based in six other Irish academic institutions: Trinity College Dublin (TCD), Dublin City University (DCU), University College Dublin (UCD), NUI Galway, University College Cork (UCC) and Waterford Institute of Technology (WIT). Operations began in October 2017 and since then, FutureNeuro has significantly increased in size. In total, there are 87 academic and clinical researchers and support staff based across these third level institutions and in the main hospitals associated with the Centre – Beaumont and St James’s Hospitals, Dublin, and Cork University Hospital.

FutureNeuro is a unique, multidisciplinary and inter-institutional research centre focusing on epilepsy, motor neurone disease (MND), multiple sclerosis (MS), Parkinson’s disease, and rare pediatric disease, and performing basic, applied and translational research in the area of diagnosis, therapeutics and eHealth. Their work is focused in partnership with the health service, patient organisations and industry to make breakthrough discoveries on the causes of brain disease
and the development of innovative technological solutions that help with diagnosis, treatment, and management.
FutureNeuro’s scientific strategy has focused on:
Developing stratification tools that facilitate diagnosis and clinical trials;
Discovery and validation of biomarkers for point-of-care diagnostics;
Application of genomic testing and pharmacogenomics to deliver precision medicine;
Bringing innovative and diseasemodifying therapeutic leads into preclinical development;
Maximising adoption of eHealth-e nabled care and research including ‘big data’ and artificial intelligence (AI).
Some achievements during phase one of the centre include: (2017-present)
180 original publications including breakthroughs in diagnostics (discovery of novel class of circulating biomarkers and technology for their detection), therapeutics (new RNA metabolism pathways, potent disease-modifying therapies and their mechanisms of action) and eHealth (applying innovative technological solutions for self-monitoring of chronic disease).
Training of 19 PhDs, 17 postdoctoral fellows (of which five started their own laboratories).
Investigator pool growth from 11 to 23 and from 12 to 48 research projects.
Leadership of eight international consortia including TRICALS, EPIXCHANGE.
Industry
Working with the leading companies in neurology is critical to the Centre’s impact. During 2021, FutureNeuro worked collaboratively with multiple industry partners including Roche, UCB, Janssen, and Congenica. The projects address a range of topics including improved bloodbased diagnostics, preclinical testing of new molecules to treat seizures, and ambulatory seizure monitoring.
Scientific highlights in 2021
Despite the impact of Covid on bench and clinical research, 2021 was another busy and successful year for FutureNeuro, with a number of important scientific breakthroughs. FutureNeuro is closely integrated into the national clinical neurology network, both adult and paediatric. This has facilitated access to key neurologists that have been critical to the success of the Centre and in turn has brought direct benefit to diagnostics and care. Both SFI-funded platform and industry research projects (eg, Congenica) led by Prof Gianpier Cavalleri and Prof Norman Delanty and through the work of Dr Katherine Benson have supported genomic clinical diagnosis in over 230 people, which has had a significant impact for these individuals and their families.
Elevated blood purine levels as a biomarker of seizures and epilepsy
Dr Tobias Engel and his team at RCSI, together with researchers in UK, Germany and clinical colleagues in Beaumont Hospital, identified a potential new biomarker that could lead to the diagnosis and detection of epilepsy via a novel, user-friendly pointof-care device, which requires a drop of blood and gives results within minutes. The
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 36
discovery was made by measuring blood purine concentrations using a point-of-care diagnostic technology based on the summated electrochemical detection of adenosine.
Measurements of blood purine concentrations were carried out using finger prick samples from preclinical models and in videoelectroencephalogram (EEG)-monitored adult patients with epilepsy. The paper is published in Epilepsia at: https://onlinelibrary.wiley.com/ doi/full/10.1111/epi.16839.
Identifying new mutations a ssociated with early-onset dementia
Dr Matthew Campbell and his research team in TCD identified previously unreported mutations in a gene called colony stimulating factor-1 receptor (CSF-1R) in an ultra-rare form of Alzheimer’s disease. This discovery may lead to better understanding of how Alzheimer’s and other dementias occur. Read the full study published in Embo Molecular Medicine at www.embopress.org/doi/ full/10.15252/emmm.202012889.
FutureNeuro epilepsy clinical network pivot to telecare during Covid-19
Before the onset of the Covid-19 pandemic, telemedicine was already an important part of the FutureNeuro Centre. Building on the HSE eHealth Ireland-funded epilepsy Lighthouse project, FutureNeuro researchers developed a pilot ePortal, allowing people to access and co-author their own epilepsy care records. The redeployment of staff to Covid-19-care and the closure of outpatient services created an urgent need to provide safe remote patient care. With access to patient-co-authored records within the National Epilepsy Electronic Patient Record (EPR), Profs Colin Doherty (St James’s Hospital) and Norman Delanty (Beaumont Hospital) moved 1,600 patient clinics online using a mixture of telephone and virtual appointments. Research by the FutureNeuro eHealth team into the facilitation of tele clinics demonstrated no loss of care contact for patients with epilepsy, and the patient survey showed that telemedicine is seen as an effective and satisfactory method of delivering chronic outpatient care. This
paper was published in Epilepsy Behaviour, and can be access here: www.epilepsybehavior. com/article/S1525-5050(20)30855-6/fulltext.
“The Irish National Epilepsy Electronic Patient Record (EPR) and the subsequent development of the electronic patient portal (ePortal) have facilitated changes in patients’ care pathways and improved patient-clinician contact and has engendered greater patient selfmanagement (Power et al, 2020). These structures provide Irish policymakers with a template for expanding an EHR to other patient populations, and ultimately to establish a national EHR.”
In addition to this, in June last year, the Economic and Social Research Institute (ESRI) published the report Advancing a Digital Healthcare Future for Ireland citing the work of FutureNeuro, which can be accessed at: www.esri.ie/publications/ developments-in-healthcare-informationsystems-in-ireland-and-internationall y.
Prediction of caregiver quality-of-life in amyotrophic lateral sclerosis (ALS) using explainable machine learning Dr Catherine Moone and PhD Candidate Anna Markella Antoniadi both from UCD and Prof Orla Hardiman (TCD), published a study in Scientific Reports on the identification of the predictors of a caregiver’s quality-of-life. In addition to the development of a model for clinical use, which would alert clinicians when a caregiver is at risk of experiencing low quality-of-life. The data was collected through the ALS Registry and via interviews with 90 patient and caregiver pairs at three time-points. Study available here: www.nature.com/articles/s41598-021-91632-2.
Building capacity to tackle neurological disease NeuroInsight
Tackling neurological disease remains FutureNeuro’s number one priority. Over a four-year period, the NeuroInsight MarieSklodowska Curie Fellowships programme will train 33 research fellows who conduct projects combining neuro and data. They
will gain practical experience in hospitals and industry. The programme will facilitate high quality research, provide opportunities to interact with clinicians, patient groups and datasets, and establish a talented group of future research leaders. To find out more and how to apply, visit www.neuroinsight.eu.
Empower
In October 2021, the Empower Data Governance Programme which was cocreated by FutureNeuro was launched. As a health research centre, Empower will create a community of practice involving patients, their carers, clinicians, statutory bodies, industry and researchers to explore how and why patient data is used for healthcare improvement and research, and develop a culture that promotes the trustworthy use of data, to facilitate collaborative, transparent and citizen-centric opportunities for the safe and ethical use of health data.
Empower will harness the collective research capabilities across four participating SFI Centres – FutureNeuro, ADAPT, Insight, and Lero (programme lead). The programme will address many different types of data ecosystems, with health data being the prime focus of FutureNeuro. See more information at www.futureneurocentre.ie.
Education and public engagement
Education and public engagement is a key focus for the entire FutureNeuro team. We have successfully partnered with NGOs such as Epilepsy Ireland to deliver a series of nationwide Epilepsy in English workshops addressing sensitive topics such as sudden unexpected death in epilepsy (SUDEP), temporal lobe epilepsy (TLE), gene therapy and managing epilepsy. We are prioritising public and patient Involvement in our research. With the appointment of a part-time PPI engagement expert, we are currently establishing a Patient Advisory Council, representing both adult and pediatric patients with a lived experience of MS, MND and epilepsy.
For more information on the work of FutureNeuro go to www.futureneurocentre.ie.

37 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
Exercise prescription for Parkinson’s – how the little details make BIG impacts
CASE REPORT
A 51-year-old male presented for a clinical exercise prescription (August 2020), having been referred by his consultant neurologist. The patient was diagnosed with Parkinson’s disease (PD) in August 2017. In the years preceding diagnosis, commonly referred to as the prodromal stage of the disease, the patient initially presented to his GP with insomnia (since confirmed as an REM disorder), constipation, depression, and anxiety. He developed a mild tremor in his right hand in early 2017 and was subsequently referred to a consultant neurologist. He is currently classified as stage 2 on the Hoehn and Yahr scale, a commonly used system for describing how the symptoms of PD progress, meaning he has unilateral involvement only, with minimal functional impairment. He had a difficult period in terms of low mood when originally diagnosed.
The exact cause of Parkinson’s disease (PD) is unknown. However, ageing, genetics, and our environment are all likely to play a role as composite factors. It is uncommon that the disease is diagnosed before the age of 50 years, but the incidence increases five-to-10 fold from the ages of 60-to-90 years.
PD is a chronic, progressive neurological disorder characterised by signs and symptoms such as bradykinesia, hypokinesia, resting tremor, rigidity, postural instability, and difficulties with gait. PD is a form of Parkinsonism,
However, he reported working through these issues and described his mental health as stable. On presentation for an exercise programme his primary concerns were weight gain (centrally), some cervical and lumbar spine discomfort, and a perceived loss of power in his golf swing. He was particularly concerned that the deterioration in his golfing performance was due to a ‘global’ loss of strength secondary to a progression in his PD.
Prior to his clinical exercise intervention, the patient did no formal exercise other than casual walking and a weekly round of golf. Due to reduced arm swing and some deterioration in gait quality he had noticed that a round of golf took him approximately 20-to-30 minutes longer compared to pre-diagnosis.
The patient is currently employed as a civil engineer. When first
which is an umbrella term for other neurodegenerative conditions including multiple system atrophy, progressive supranuclear palsy, Lewy body dementia, and corticobasal degeneration. These Parkinsonism conditions are typically referred to as atypical Parkinsonian disorders, with similar core features to PD, yet varying clinical signs that lead to differential diagnoses. The most commonly observed motor deficits associated with PD are due to degenerative change in the dopaminergic nigrostriatal pathway of the midbrain. In
diagnosed, he was anxious to keep the information private – being primarily concerned at how his competency levels may be perceived. However, he has since disclosed this information to his employer, who has proven very supportive and reassuring. During his initial assessment, he subjectively described difficulties with activities of daily living (ADLs). Objectively, there was a generalised reduced amplitude in movement, notably gait cadence, arm swing, micrographia (handwriting), touch and scroll usage of his laptop, and difficulty with fine motor tasks (such as buttoning his shirt before going to work). The patient had no inclination that these ‘smaller’ issues could be improved by exercise. He has two teenage daughters. He is motivated to maintain a good qualityof-life and reduce the impact or severity of PD where possible. He has a good relationship with his GP and neurologist.
a PD patient there is a resultant reduction in the amount of dopamine produced. Inflammation and mitochondrial dysfunction also contribute to the disease process. The progression of the disease is succinctly described by the Hoehn and Yahr (HY) staging scale ( Figure 1).
Ongoing medical management
Currently the case report patient in this article is taking Sinemet 25mg, a levodopacarbidopa combination medication. The levodopa changes into dopamine upon entering the brain, which most noticeably
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 38
AUTHORS: Marion Slattery, Occupational Therapist and Clinical Exercise Specialist, Personal Health – Medical Exercise Clinic, Rathmines, Dublin; and Andrew Dunne, Chartered Physiotherapist and Clinical Exercise Specialist, Personal Health – Medical Exercise Clinic, Rathmines, Dublin
has an effect on his resting tremor. From a musculoskeletal perspective he also feels that it alleviates some cervical and lumbar stiffness. The carbidopa component may have helped to reduce some unpleasant side-effects, such as nausea when first prescribed Sinemet. To this end the patient no longer experiences these symptoms. The patient is also taking rasagiline (0.5mg), a monoamine oxidase-B (MAO-B) inhibitor. The MAO-B enzyme is a catalyst that triggers a chemical reaction, ultimately preventing dopamine levels from getting too high in a person. Therefore an MAO-B inhibitor prevents this process happening in a PD patient who requires increased dopamine. Caution and vigilance is encouraged around how rasagiline can interact with some commonly-used prescription and over-the-counter medications.
The patient was prescribed fluoxetine by his GP to help manage low mood, which has proven effective. Additional medications include melatonin for disturbed sleep and occasionally a short-term course of
oral non-steroidal anti-inflammatories (NSAIDs) for cervical and lumbar discomfort. Finally, the patient takes a stool softener (senna) as required.
He was referred by his GP for MRI imaging at cervical and lumbar levels on separate occasions in the last 18 months. Overall the reports were non-remarkable, suggesting mild degenerative disc disease at C3-4, C4-5, L4-5, L5-S1 levels, with no evidence of canal stenosis or narrowing at exit foramina bilaterally. On his most recent neurology appointment he was referred for a clinical exercise programme, specifically to address general movement and fine motor deficits which had recently become impactful at work.
Exercise prescription as part of the medical treatment plan
The most recently published (highquality) peer-reviewed literature is suggesting amplitude of movement ought to be a primary focus in PD exercise prescription. These advances in exercise specificity are having a direct impact
on clinical signs and features of the condition, in the same way medication has been impactful to date.
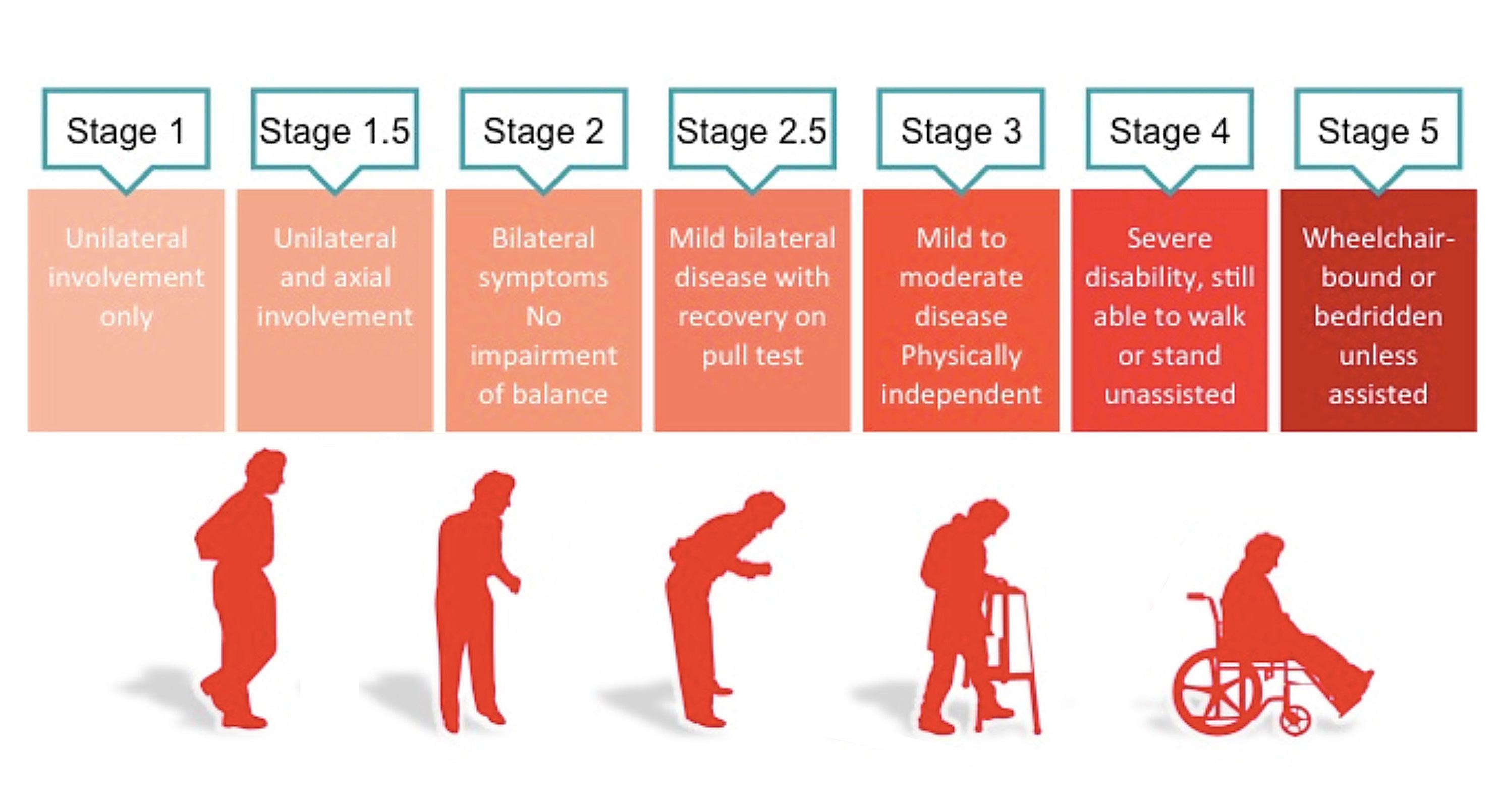
In plain language, the exercises ought to have a greater focus on quality and amplitude of movement (as opposed to generic strength and conditioning) in a bid to enhance this patient’s handwriting, laptop usage, self-dressing, and walking, which are essential to his sense of wellbeing. According to the American College of Sports Medicine (ACSM) guidelines (2021), “ultimately the exercise prescription in this case should appear to slow the rate of disease progression.”
Rigorous measurement of neuromotor development is a challenge for the exercise specialist and neurologist alike.
In this regard, accurate observation and functional comparisons are deemed sufficient. Secondary considerations ought to include the ACSM ‘FITT’ guidelines to best address cardiorespiratory fitness (CRF), flexibility, muscular strength and endurance in the PD patient.
39 Psychiatry and Neurology | Volume 8 | Issue 1 | 2022
F IGURE 1: Hoehn and Yahr Scale
How do I make my exercise prescription specific?
With amplitude of movement prioritised, it is now worth adding specificity to the exercise prescription. The Lee Silverman Voice Training (LSVT) BIG programme is an exercise treatment consisting of large amplitude movements and exaggerated movement patterns (Figure 2). The exercises are performed with high intensity and effort that becomes progressively more difficult and complex, with the overall goal of restoring ‘normal’ movement amplitude in real-life situations. This programme results in ‘moments of calibration’ as it were, whereby normal pre-Parkinson’s movement patterns are restored.
LSVT BIG has been proven effective for motor function impairments in people with PD, when compared to control groups (performing generic, aerobic and resistance exercise programmes). Other relevant specific exercise programmes exist, including PD Warrior.
In general, if a clinician is embarking on a PD exercise programme with a patient, it needs to include a variety of challenging physical activities (eg, multidirectional step training, step up and down, reaching forward and sideways with maximal speed and effort, obstacle courses, turning in standing and supine). These exercises demand an intensive neuroactive response, promoting neuroplasticity, dual tasking, balance and coordination. It is incumbent on the clinician to have ‘had their Weetabix’ as regular demonstration, rhythmic auditory, and verbal cueing is a vital part of the process (anecdotally we can report these workouts are also highlevel intensity for non-PD patients).

Resistance training is recommended twice weekly to avoid secondary complications of PD such as muscle wastage. Free weights can be used in the case of this article’s patient due to his mild/moderate presentation. At more advance stages of the disease, overhead resistance training with free weights can become unsafe due to increased severity of tremor. Therefore,
weight machines and other resistive devices (such as pulleys and resistance bands) may be safe alternatives to free weights. At all stages of PD, lower limb strength training is indicated, with modifications dependent on presentation. Attention should be given to extensor muscles of the trunk and hip to counteract postural decrements.
Continuous aerobic exercise can challenge even the most motivated athletes; therefore the modality should depend on patient
preferences, with an emphasis on enjoyment if possible. If the patient enjoys the aerobic components of the programme, it is far more likely to become a consistent part of their lifestyle. In this regard, anything from treadmill, elliptical trainer, recumbent bicycle, aqua aerobics, outdoor hill walking, tango, or waltz dancing are all evidencebased interventions for aerobic benefit.
Finally, flexibility and range of motion (ROM) exercises can be active (patient alone) or passive (clinician assisted). Typically there is an emphasis on spinal mobility and axial rotation. In this case the patient included a daily cervical, thoracic and lumbar mobility routine incorporating Tai Chi type movements throughout, with the assistance of a guided DVD.


Case report patient update
The patient has worked intensively for 15 months on a hybrid exercise programme. Body composition has changed with a small increase in lean muscle mass, and a cumulative weight loss of 7kg. He has reported significant improvement in ADLs, such as shirt buttoning, laptop usage, handwriting, reaching, and rotating in general. Most importantly for the patient, he has regained some speed and torque in his golf swing, and is also able to keep up with the pace of his peers in between shots. His neurologist has encouraged him to remain as active as possible.
Summary and recommendations
On presentation for an exercise programme, the case report PD patient had no inclination that some of the clinical features of Parkinson’s could be addressed through exercise specificity. These neuromotor changes proved to be a significant source of motivation, renewed vigour and confidence for the participant. An exercise prescription needs to be as equally specific as a medical prescription, in terms of frequency, intensity, duration, dosage and type. In modern medicine it is vital that exercise prescription is included as a key part of the medical treatment plan. ■
References on request
Volume 8 | Issue 1 | 2022 | Psychiatry and Neurology 40
F IGURE 2: Examples of LSVT BIG exercises (Source: www.lsvtglobal.com/LSVTBIG)
Because ON TIME is their time1
You can offer your patients continuous dopaminergic stimulation with Duodopa®1,2


PRESCRIBING INFORMATION:
Duodopa 20 mg/ml + 5 mg/ml intestinal gel (levodopa/carbidopa)
Refer to Summary of Product Characteristics (SmPC) for full prescribing information.
Presentation: Intestinal gel containing 20mg/ml levodopa and 5mg/ml carbidopa monohydrate.
Indication: Advanced levodopa-responsive Parkinson’s disease with severe motor fluctuations and hyperkinesia or dyskinesia when available combinations of Parkinson medicinal products have not given satisfactory results. Dosage and Administration: Adults/Elderly: Administration by portable pump directly into the duodenum or upper jejeunum via a percutaneous endoscopic gastrostomy (PEG) or radiological gastrojejunostomy tube. Initially a nasoduodenal/nasojejunal tube should be considered to determine patient’s response before a PEG-J tube is placed. Where the physician considers this assessment is not necessary, the nasojejunal test phase may be waived and treatment initiated directly with placement of PEG-J. Duodopa is given initially as monotherapy and dose adjusted to optimal response for the individual patient. Total dose/day is composed of three individually adjusted doses: morning bolus, continuous maintenance and extra bolus doses administered over approximately 16 hours. Total morning dose usually 5-10ml (100-200mg levodopa) but not exceeding 15ml (300mg levodopa). Continuous maintenance dose should be between 1-10ml/hr (20200mg levodopa/hr) but usually 2-6ml/hr (40-120mg levodopa/hr). Maximum recommended daily dose is 200ml. Extra bolus doses (if patient becomes hypokinetic during the day) are normally 0.5-2.0ml. Increase maintenance dose if more than 5 extra bolus doses/day are needed. Fine adjustments to the morning bolus, maintenance and extra bolus doses should be made over a few weeks after the initial dose setting. Sudden deterioration in response with recurring motor fluctuations indicates tube may have moved from duodenum/ jejunum into stomach and needs repositioning. Medicine cassettes are for single use only and should not be used for longer than 24 hours, even if some medicinal product remains. Treatment is usually administered during the patient’s awake period. If medically justified, Duodopa may be administered for up to 24 hours. Opened cassettes should not be reused. Children: No relevant use in the paediatric population. Renal/hepatic impairment: No studies on the pharmacokinetics of carbidopa and levodopa in patients with hepatic or renal impairment. Dose titration should be conducted with caution in patients with severe renal and hepatic impairment. Contraindications, Warnings, Precautions etc: Contraindications: Hypersensitivity to ingredients, narrow-angle glaucoma, severe heart failure or cardiac arrhythmia, acute stroke. Conditions where adrenergics are contraindicated (e.g. pheochromocytoma, hyperthyroidism, Cushing’s syndrome). Nonselective MAO-inhibitors and selective MAO type A inhibitors are contraindicated and should be withdrawn at least two weeks before starting Duodopa. Duodopa should not be used in patients with suspicious undiagnosed skin lesions or a history of melanoma. Warnings/Precautions: Not recommended for drug-induced extrapyramidal reactions. Caution in severe pulmonary or cardiovascular disease, bronchial asthma, renal, hepatic or endocrine disease, or history of peptic ulcer disease or of convulsions, past or current psychosis, chronic wide-angle glaucoma, co-administration with antipsychotics with dopamine receptor blocking properties or with medicines which may cause orthostatic hypotension. In patients with a history of myocardial infarction who have residual nodal or ventricular arrhythmias, cardiac function should be monitored with care during initial dose adjustments. Monitor all patients for development of mental changes, depression with suicidal tendencies and other serious mental changes. Neuroleptic Malignant like Syndrome with secondary rhabdomyolysis has not been reported with Duodopa but may occur on abrupt dose reduction/withdrawal. Periodically evaluate hepatic, haematopoietic, cardiovascular and renal function during extended therapy. Increases in impulse control disorders have been reported and patients should be monitored and reviewed.
Patients and providers are advised to monitor for melanomas on a regular basis when using Duodopa. Ideally, periodic skin examinations should be performed by dermatologists. Dose may need to be adjusted downwards to avoid levodopa induced dyskinesia. Sudden or gradual worsening of bradykinesia may indicate an obstruction in the device and should be investigated. Duodopa contains hydrazine, a degradation product of carbidopa that can be genotoxic and possibly carcinogenic, clinical significance of exposure unknown. Reported complications in clinical studies include abscess, bezoar, ileus, implant site erosion/ulcer, intestinal haemorrhage, intestinal ischaemia, intestinal obstruction, intestinal perforation, intussusception, pancreatitis, peritonitis, pneumonia (including aspiration pneumonia), pneumoperitoneum, post-operative wound infection and sepsis. Before initiation of treatment, patients and caregivers should be warned of the potential risk of developing Dopamine Dysregulation Syndrome (DDS). Polyneuropathy has been reported in patients treated with levodopa/carbidopa intestinal gel. Before starting therapy evaluate patients for history or signs of polyneuropathy and known risk factors, and periodically thereafter. Drug Interactions: Antihypertensives, tricyclic antidepressants, anticholinergics, dopamine receptor antagonists, benzodiazepines, isoniazide, phenytoin, papaverine, sympathicomimetics, iron, protein-rich diet, COMT inhibitors (e.g. tolcapone, entacapone) amantadine. Duodopa dose adjustment may be needed when used with these drugs. Duodopa can be taken with MAO type B inhibitors (e.g. selegiline) although serious orthostatic hypotension may occur and the dose of levodopa may need to be reduced. Fertility, Pregnancy and Lactation: Limited data relating to the use of levodopa/carbidopa in pregnant women. Duodopa is not recommended during pregnancy. Breast-feeding should be discontinued during treatment with Duodopa. No adverse reactions on fertility have been observed in preclinical studies with carbidopa or levodopa alone. Ability to Drive and Operate Machinery: Caution; Duodopa can have a major influence on the ability to drive and use machines. Refrain from driving/operating machinery if somnolence and/or sudden sleep episodes occur. Side Effects: Very common: Weight decreased, Anxiety, Depression, Insomnia, Dyskinesia, Parkinson’s disease, Orthostatic hypotension, Nausea, Constipation, Fall, Common: Anaemia, Increased weight, Amino acid level increased (Metylmalonic acid increased), Blood homocysteine increased, Decreased appetite, Vitamin B6 & B12 deficiency, Abnormal dreams, Agitation, Confusional state, Hallucination, Impulsive behaviour, Psychotic disorder, Sleep attacks, Sleep disorder, Dizziness, Dystonia, Headache, Hypoaesthesia, On and off phenomenon, Paraesthesia, Polyneuropathy, Somnolence, Syncope, Tremor, Heart rate irregular, Hypertension, Hypotension, Dyspnoea, Oropharyngeal pain, Abdominal distension, Diarrhoea, Dry mouth, Dysgeusia, Dyspepsia, Dysphagia, Flatulence, Vomiting, Dermatitis contact, Hyperhidrosis, Oedema peripheral, Pruritus, Rash, Muscle spasms, Neck pain, Urinary incontinence, Urinary retention, Fatigue, Pain, Asthenia. Device and Procedure Related Adverse Reactions: Very common: Postoperative wound infection, Abdominal pain, Excessive granulation tissue, Complications of device insertion, Incision site erythema, Post procedural discharge, Procedural pain, Procedural site reaction. Common: Incision site cellulitis, Post procedural infection, Abdominal discomfort, Abdominal pain upper, Peritonitis, Pneumoperitoneum, Pneumonia/Aspiration pneumonia, Device dislocation, Device occlusion, Gastrointestinal stoma complication, Incision site pain, Postoperative Ileus, Post procedural complication, Post procedural discomfort, Post procedural haemorrhage. Laboratory values: May change. Prescribers should consult the SmPC for the complete list of reported side effects. HCPs are asked to report any suspected adverse reactions via HPRA Pharmacovigilance; website: www.hpra.ie. Marketing Authorisation Number: PA 1824/2/1. Legal Category: POM (S1B). Further information is available from: AbbVie Limited, 14 Riverwalk, Citywest Business Campus, Dublin 24. Date of Revision: January 2021. PI/2/005
References: 1. Duodopa® Summary of Product Characteristics, available on www.medicines.ie 2. Nyholm D. The rationale for continuous dopaminergic stimulation in advanced Parkinson’s disease. Parkinsonism Relat Disord. 2007;13(suppl):S13-S17. doi:10.1016/j.parkreldis.2007.06.005.
IE-DUOD-210040.
Date of Preparation: September 2021.
In the treatment of advanced Parkinson’s disease
Duodopa® is indicated for the treatment of advanced levodoparesponsive Parkinson’s disease with severe motor fluctuations and hyperkinesia or dyskinesia when available combinations of Parkinson medicinal products have not given satisfactory results1
People
in this piece are models, not actual
patients.


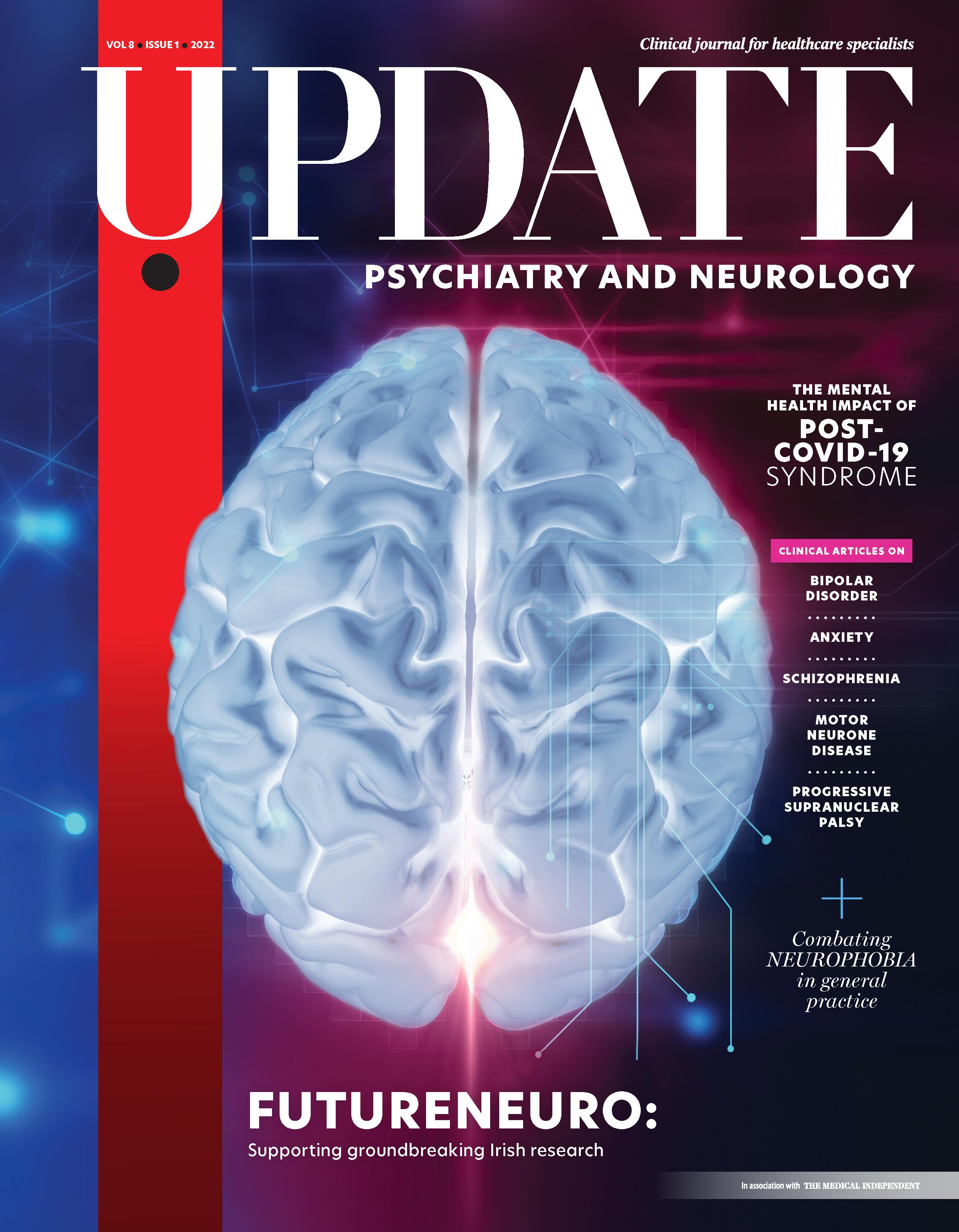



 ALL REPORTS BY VALERIE RYAN
ALL REPORTS BY VALERIE RYAN